| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://jnr.elmerpub.com |
Case Report
Volume 15, Number 2, March 2025, pages 83-86
A Case Report of Parkinsonism Following Dengue Infection
Theodore Amadeo Nathana, c , Raisa Wibowoa, Debora T. Butarbutarb
aEmergency Department, Fatima Hospital, Ketapang, Kalimantan Barat, Indonesia
bNeurology Department, Fatima Hospital, Ketapang, Kalimantan Barat, Indonesia
cCorresponding Author: Theodore Amadeo Nathan, Emergency Department, Fatima Hospital, Ketapang, Kalimantan Barat, Indonesia
Manuscript submitted September 17, 2024, accepted January 18, 2025, published online January 25, 2025
Short title: Parkinsonism Post Dengue Infection
doi: https://doi.org/10.14740/jnr855
| Abstract | ▴Top |
Dengue fever is one of the most common viral infections found in tropical countries. Parkinsonism, a complication of dengue fever, is relatively new, and only a handful of cases have been documented. A 32-year-old female developed tremors and bradykinesia on the left side of her body 1 day after discharge following dengue fever. Alternative etiologies were excluded by imaging and laboratory testing. A week-long regimen of levodopa 100 mg three times a day (TID) resulted in a marked improvement in her symptoms. Neurological complications such as parkinsonism are uncommon in dengue virus infections. Current theories suggest that neurotropic invasion through the brain or immune-mediated mechanisms are responsible. This report represents Indonesia’s first account of parkinsonism following dengue infection. Such cases are valuable for expanding the list of neurological complications.
Keywords: Parkinsonism; Dengue infection; Treatment
| Introduction | ▴Top |
Dengue fever is one of the most common viral infections found in tropical regions [1]. The diagnosis of dengue virus (DENV) infection in Indonesia is made through clinical presentation, laboratory findings, and serology testing. Specific laboratory confirmation methods are seldom used [2].
Rarely, atypical manifestations present as neurological complications. Dengue encephalopathy, dengue encephalitis, ocular manifestations, dengue-associated stroke, immune-mediated neurological syndromes, and neuromuscular complications make up the spectrum [3]. One peculiar manifestation is parkinsonism, a relatively new finding [4, 5]. Only eight cases have been published at present.
| Case Report | ▴Top |
Investigations
A 32-year-old female with no previous history of neurological deficit presented to the neurology outpatient clinic with involuntary tremors on the left side of her body.
She was admitted to the emergency room 8 days prior with a 4-day history of high-grade fever, myalgia, arthralgia, headaches, and decreased appetite. She was fully conscious, and oriented. Her vital signs were normal, apart from a temperature of 39.2 °C, and tachycardia. Physical and neurological examination revealed no signs other than abdominal pain. A blood test revealed leukopenia (3.3 × 109/L), and borderline thrombocytopenia (167 × 109/L). Other laboratory tests were normal. Dengue nonstructural protein 1 antigen (NS-1) was positive, but immunoglobulin (Ig)M and IgG were negative for DENV. A diagnosis of dengue fever was made, due to outbreaks in the alleged area, and the patient was treated with intravenous fluids and supportive therapy. Throughout her stay, she developed no focal or global neurological deficits. Her symptoms gradually subsided, and she was discharged on her sixth day of treatment. Another blood test was taken before her discharge, which revealed thrombocytopenia (94 × 109/L).
She awoke the following morning with tremors on the left side of her body, and muscle twitching in the left face. Tremors were more strongly felt at rest. She had slow movements, accompanied by slurring speech, and short-term memory impairment. Consumption of antipsychotic or anti-emetic drugs, and exposure to heavy metals and industrial toxins were denied. A Montreal Cognitive Assessment-Indonesian Version (MoCA-INA) revealed an overall score of 26/30. Cranial nerve examination displayed dysarthria. Muscle strength was intact, with normal deep tendon reflexes, and no pathological reflexes. There was a resting tremor on both the left arm and leg, and bradykinesia was evident during the finger tapping test, toe-tapping test, fist open-close test, and supination-pronation test (Supplementary Material 1, jnr.elmerpub.com). Coordination and sensory examinations were normal.
Diagnosis
A repeat blood count showed normal values, and additional screening for human immunodeficiency virus (HIV) antigen provided nonreactive results. Head computed tomography (CT) scan showed normal findings (Fig. 1). Unfortunately, electromyography (EMG), magnetic resonance imaging (MRI) and cerebrospinal fluid (CSF) analyses were not available due to limited resources.
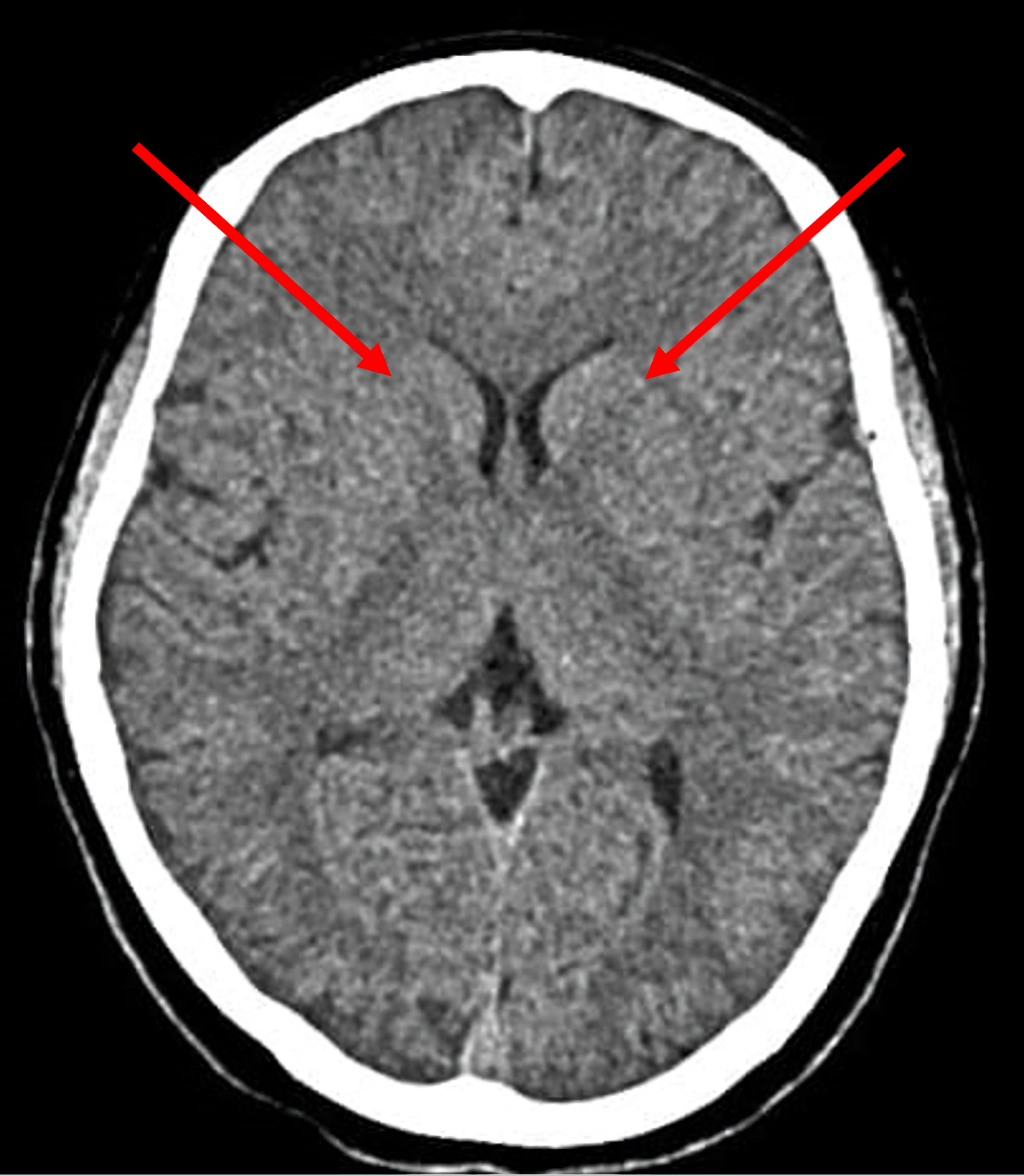 Click for large image | Figure 1. Non-contrast head CT with arrows (red) revealing no abnormalities in the region of the basal ganglia. CT: computed tomography. |
Treatment
A diagnosis of parkinsonism post-dengue infection was made, and she was treated with trihexyphenidyl, 2 mg twice a day (BID) for 1 month. She returned as scheduled, claiming her symptoms had persisted. Her regimen was then altered to levodopa, 100 mg three times a day (TID) for 7 days.
Follow-up and outcomes
On follow-up, she acknowledged marked improvement in her symptoms. Her speech was normal, her tremors’ intensity decreased, and she no longer experienced twitching. However, her movements remained slow.
| Discussion | ▴Top |
Parkinsonism following DENV infection is rare. A thorough search of PubMed, with the terms “dengue” and “parkinsonism”, generated eight case reports of parkinsonism associated with DENV infection. The first was discovered in Malaysia in 2013, with the most recent report published in 2023, from India [5, 6].
The criteria for DENV-associated parkinsonism are based on a clinical diagnosis of a DENV infection with concurrent laboratory findings and a diagnosis of parkinsonism during or immediately after DENV infection [4]. The Movement Disorder Society (MDS) defines parkinsonism as the presence of bradykinesia with resting tremor, or rigidity [7]. Bradykinesia is established using the finger-toe tapping test. Rest tremor is defined as a tremor in the fully resting limb; however, it can also be observed with prolonged posture [7]. In this case, the patient had high-grade fever, accompanied by typical DENV symptoms, with concurrent laboratory findings, during a period of dengue outbreak. The negative result of IgM may have been due to the premature timing of the test, as antibodies appear near the end of the first week [1]. The patient developed bradykinesia, and resting tremor, 1 day after being discharged, meeting the aforementioned criteria. Insignificant brain imaging and nonreactive anti-HIV antibodies excluded vascular etiologies, head trauma, brain malignancy, normal-pressure hydrocephalus and HIV infection. Drug and toxin-induced parkinsonism was also excluded.
Of the eight reported cases, six developed parkinsonism along with dengue encephalopathy or encephalitis. The emergence of movement disorders in these cases was attributed to direct neurotropic invasion of DENV into the central nervous system (CNS). This was strengthened by MRI findings of the “double doughnut” sign, and in one report, positive IgM on CSF analysis. However, MRI findings of dengue encephalitis tend to be nonspecific, and significant findings are more commonly observed in Japanese encephalitis virus or herpes simplex virus encephalitis [8]. The remaining two studies did not show signs of severe dengue, and both laboratory and imaging results were equally unremarkable [5, 9]. Our case adopts similar traits to the latter two studies, in which parkinsonism developed during the convalescent phase of DENV infection, suggesting that this was immune-mediated. Bradykinesia and resting tremor were the most frequent symptoms, which was consistent with our case. Our patient demonstrated slurred speech but did not exhibit signs of rigidity, hypomimia or postural instability. Some studies have reported more unusual movement disorders, such as stereotypy and rapid lingual tremor [4, 10]. Our patient suffered short-term memory impairment, signifying possible involvement of the hippocampus. Parkinsonism is linked to a decrease in dopamine production as a result of neuronal damage [7]. The immune mechanism involved is theorized to be the blockade of the interferon-1 pathway by DENV, which triggers mitochondrial dysfunction in the brain, and neuronal death. Viral activation may lead to hypercytokinemia and aggregation of microglia surrounding dopaminergic neurons, causing neuroinflammation [10].
Treatment is centered around dopaminergic agents and immunosuppressors. Previous reports have shown ideal outcomes following administration of levodopa and corticosteroids [9-11]. Our patient had markedly diminished symptoms following a 1-week course of levodopa 100 mg TID after a previously failed attempt with trihexyphenidyl. This report represents Indonesia’s first account of parkinsonism following dengue infection due to suspected immune-mediated mechanisms. Such cases are valuable for expanding the list of neurological complications.
A significant limitation of this case report is the lack of a positive IgM serology test for dengue infection, which could have substantiated the diagnosis. Additionally, due to our hospital’s location in a rural area, we did not have access to advanced diagnostic tools such as EMG, MRI, and CSF analyses, which could have provided valuable insights into the underlying pathophysiology of parkinsonism following dengue infection. Referral to a more advanced health center was not pursued, as the patient showed marked clinical improvement in response to a 1-week course of levodopa. This improvement reduced the urgency for further diagnostic evaluation. Despite these limitations, we believe the case provides valuable insights into a rare neurological complication of dengue infection and underscores the need for future studies with access to more comprehensive diagnostic modalities to elucidate the mechanisms involved.
Learning points
Neurological complications such as parkinsonism are uncommon in DENV infections. Current theories suggest that neurotropic invasion through the brain or immune-mediated mechanisms are responsible. This report represents Indonesia’s first account of parkinsonism following dengue infection.
| Supplementary Material | ▴Top |
Suppl 1. Bradykinesia was evident on finger-tapping test, toe-tapping test, fist open-close test, and supination-pronation test. A resting tremor was seen during full relaxation of the left hand.
Acknowledgments
The authors have no acknowledgements
Financial Disclosure
No external source of funding was given to this study
Conflict of Interest
No conflict of interest to declare.
Informed Consent
Written informed consent was obtained.
Author Contributions
All authors contributed equally. Concepts: TAN, RW, DTB. Design: TAN, RW, DTB. Definition of intellectual content: TAN, RW, DTB. Literature search: TAN, RW, DTB. Clinical studies: TAN, RW, DTB. Data acquisition: TAN, RW, DTB. Data analysis: TAN, RW, DTB. Manuscript preparation: TAN, RW, DTB. Manuscript editing: TAN, RW, DTB. Manuscript review: TAN, RW, DTB. Guarantor: TAN.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
DENV: dengue virus; NS-1: nonstructural protein 1 antigen; MoCA-INA: Montreal Cognitive Assessment-Indonesian Version; CT: computed tomography; MRI: magnetic resonance imaging; CSF: cerebrospinal fluid; MDS: Movement Disorder Society; CNS: central nervous system; EMG: electromyography
| References | ▴Top |
- World Health Organization. Regional Office for South-East Asia. Comprehensive guidelines for prevention and control of dengue and dengue haemorrhagic fever. World Health Organization Regional Office for South-East Asia. 2011.
- Utama IMS, Lukman N, Sukmawati DD, Alisjahbana B, Alam A, Murniati D, Utama I, et al. Dengue viral infection in Indonesia: Epidemiology, diagnostic challenges, and mutations from an observational cohort study. PLoS Negl Trop Dis. 2019;13(10):e0007785.
doi pubmed - Trivedi S, Chakravarty A. Neurological complications of dengue fever. Curr Neurol Neurosci Rep. 2022;22(8):515-529.
doi pubmed - Ganaraja VH, Kamble N, Netravathi M, Holla VV, Koti N, Pal PK. Stereotypy with Parkinsonism as a rare sequelae of dengue encephalitis: a case report and literature review. Tremor Other Hyperkinet Mov (N Y). 2021;11:22.
doi pubmed - Azmin S, Sahathevan R, Suehazlyn Z, Law ZK, Rabani R, Nafisah WY, Tan HJ, et al. Post-dengue parkinsonism. BMC Infect Dis. 2013;13:179.
doi pubmed - Kuraning K, Gupta Kv V, Murthy P, Kumar Ak A, N N, H GV. An interesting case of dengue encephalitis with parkinsonism sequela. Cureus. 2023;15(9):e44970.
doi pubmed - Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, et al. MDS clinical diagnostic criteria for Parkinson's disease. Mov Disord. 2015;30(12):1591-1601.
doi pubmed - Lnu P, Sehgal V, Bhalla Sehgal L, Gulati N, Kapila S. The spectrum of MRI findings in dengue encephalitis. Cureus. 2022;14(9):e29048.
doi pubmed - Panda PK, Sharawat IK, Bolia R, Shrivastava Y. Case report: dengue virus-triggered parkinsonism in an adolescent. Am J Trop Med Hyg. 2020;103(2):851-854.
doi pubmed - Garg D, Gupta A, Tiwari S, Sharma S. Rapid lingual tremor and parkinsonism in dengue encephalitis. Ann Indian Acad Neurol. 2023;26(4):586-587.
doi pubmed - Lee MF, Voon GZ, Lim HX, Chua ML, Poh CL. Innate and adaptive immune evasion by dengue virus. Front Cell Infect Microbiol. 2022;12:1004608.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.