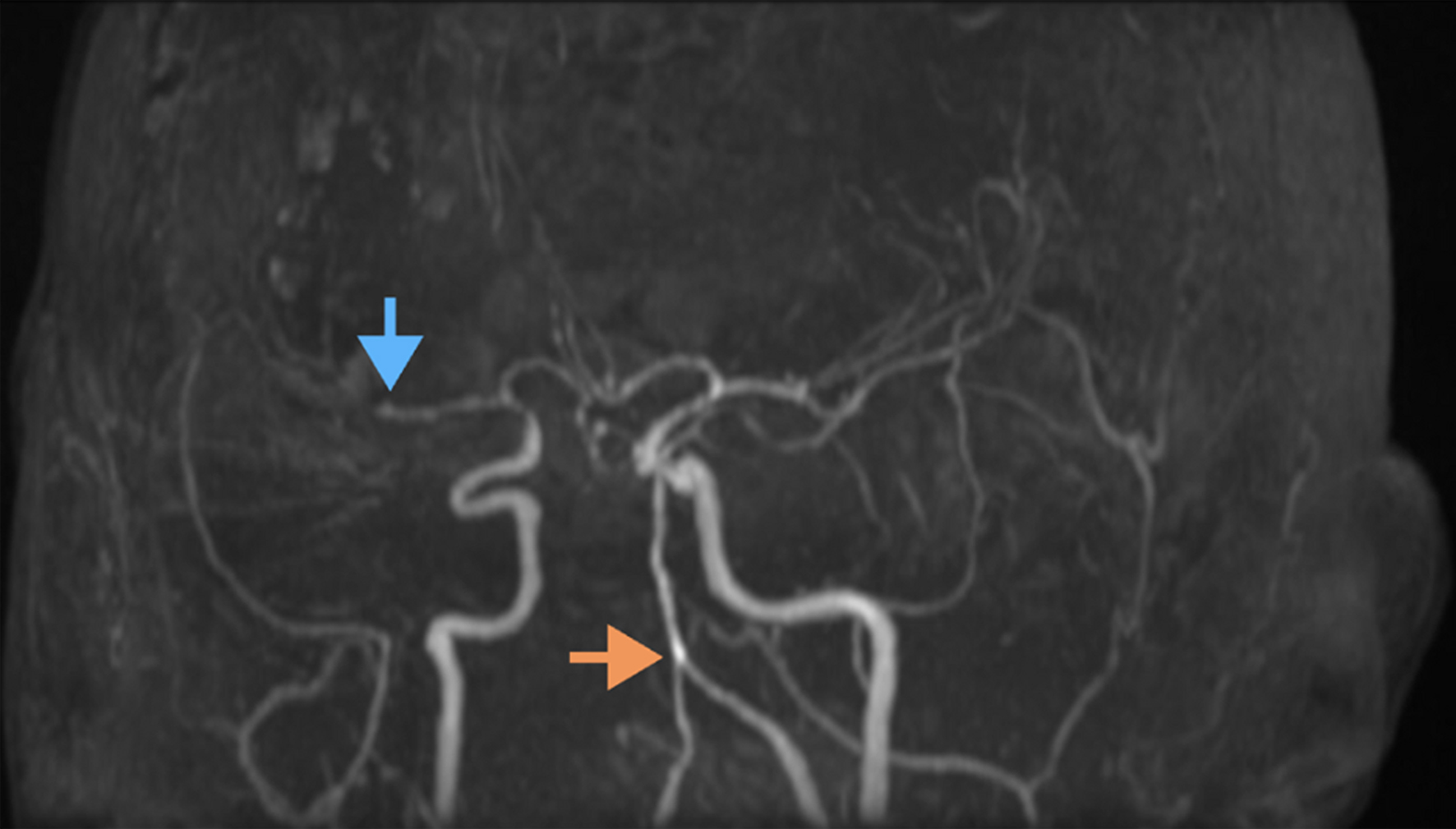
Figure 1. Magnetic resonance angiography (MRA) of the brain demonstrating vascular abnormalities. The orange arrow highlights tortuous and ectatic vertebral and basilar arteries, indicative of dolichoectasia. The blue arrow points to an occlusion of the right M2 segment of the middle cerebral artery. Additional findings include segmental narrowing and irregularity suggestive of underlying vasculopathy or vessel wall pathology.