| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://jnr.elmerpub.com |
Original Article
Volume 15, Number 1, January 2025, pages 33-38
The Role of Erythrocyte Sedimentation Rate as a Prognostic Factor in Intracerebral Hemorrhage
Ereida Rrakllia, d, Frenki Gjikab, Oneda Cibukuc
aDepartment of Neurology, Berat Hospital Center, Berat, Albania
bThe University of Buckingham, Buckingham, UK
cDepartment of Neurology, University Hospital Mother Theresa, Tirana, Albania
dCorresponding Author: Ereida Rraklli, Department of Neurology, Berat Hospital Center, Berat, Albania
Manuscript submitted October 8, 2024, accepted December 16, 2024, published online December 31, 2024
Short title: ESR as a Prognostic Factor in ICH
doi: https://doi.org/10.14740/jnr860
| Abstract | ▴Top |
Background: Intracerebral hemorrhage (ICH) is a severe type of stroke with high mortality and long-term disability rates. Early identification of patients at high risk of poor outcomes is crucial. Erythrocyte sedimentation rate (ESR), a nonspecific marker of inflammation, may serve as a prognostic indicator in ICH patients.
Methods: This retrospective cohort study analyzed 82 ICH patients from December 2021 to February 2024. Patients were divided into high ESR (≥ 20 mm/h) and normal ESR (< 20 mm/h) groups. Demographic, clinical, and laboratory data were collected, and outcomes were assessed using the modified Rankin Scale (mRS) at 6 months post-ICH. Logistic regression analyzed the association between ESR levels and outcomes.
Results: Elevated ESR was observed in 35 patients (42.7%). Mortality rate at 6 months was significantly higher in the elevated ESR group (20% vs. 8.5%, P = 0.03), with elevated ESR being an independent predictor of mortality (odds ratio (OR) = 2.5). Functional impairment (mRS > 3) was also higher in the elevated ESR group (65.7% vs. 34%, P = 0.002), with elevated ESR independently associated with functional impairment (OR = 3.1).
Conclusions: Elevated ESR at admission is an independent predictor of mortality and functional impairment in ICH patients. ESR can aid in risk stratification and guide clinical decision-making, emphasizing the role of inflammation in ICH.
Keywords: Intracerebral hemorrhage; Erythrocyte sedimentation rate; Prognostic factors; Inflammation; Clinical outcomes
| Introduction | ▴Top |
Intracerebral hemorrhage (ICH) is a severe type of stroke caused by bleeding within the brain tissue. It accounts for approximately 10-20% of all strokes and has a high rate of mortality and long-term disability. The early identification of patients at high risk of poor outcomes is crucial for tailoring appropriate interventions and improving prognosis [1-3].
Erythrocyte sedimentation rate (ESR) is a nonspecific marker of inflammation, commonly elevated in various inflammatory conditions. Previous studies have explored the role of inflammation in stroke, with markers like C-reactive protein (CRP) being linked to outcomes [4, 5]. However, there are limited data on the prognostic significance of ESR specifically in ICH patients.
This study aims to investigate whether elevated ESR at admission can serve as an independent predictor of mortality and functional outcomes in patients with ICH. Understanding this relationship could provide valuable insights into the pathophysiology of ICH and help identify patients who may benefit from more intensive monitoring and treatment.
| Materials and Methods | ▴Top |
This retrospective cohort study was conducted on 82 patients diagnosed with ICH between December 2021 and February 2024. Inclusion criteria were adult patients (aged 18 years and older) with a confirmed diagnosis of ICH via computed tomography (CT). Patients with secondary causes of ICH (e.g., trauma, aneurysm, arteriovenous malformation) were excluded from the study.
Patient data were collected from patients’ recordings, including demographic information (age, gender), clinical presentation (Glasgow Coma Scale score, ICH location and volume), comorbidities (hypertension, diabetes, atrial fibrillation), and laboratory values, including ESR levels at admission. Outcomes were assessed at 6 months post-ICH using the modified Rankin Scale (mRS) to evaluate functional status and mortality rates.
Patients were divided into two groups based on their ESR levels at admission: high ESR (greater than 20 mm/h) and normal ESR (20 mm/h or less). The primary outcomes were mortality and functional impairment, defined as an mRS score greater than 3, indicating moderate to severe disability.
Continuous variables were compared using t-tests, while categorical variables were compared using Chi-square tests. Logistic regression analysis was performed to assess the association between ESR levels and outcomes, adjusting for potential confounders such as age, gender, initial ICH volume, and comorbidities. A P value of less than 0.05 was considered statistically significant.
The protocol was approved by the relevant ethics committee. This study was conducted in full compliance with ethical standards for human participants. All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committee.
| Results | ▴Top |
Patient demographics and clinical characteristics
The study included 82 patients diagnosed with ICH, with a mean age of 65 years (range: 35 - 89 years). Among these patients, 45 were male (54.9%) and 37 were female (45.1%) [1, 2]. Elevated ESR levels (greater than 20 mm/h) were observed in 35 patients (42.7%), while 47 patients (57.3%) had normal ESR levels (Table 1) [6].
 Click to view | Table 1. Patient Demographics and Clinical Characteristics |
Patients underwent routine coagulation profiles (e.g., prothrombin time, partial thromboplastin time, platelet counts) as part of standard diagnostics. No acute traumatic ICHs secondary to hematological disorders were identified.
Mortality
The overall mortality rate at 6 months was 13.4% (11 patients). Patients with elevated ESR had a significantly higher mortality rate compared to those with normal ESR levels (20% vs. 8.5%, P = 0.03) [7]. Logistic regression analysis revealed that elevated ESR was an independent predictor of mortality (odds ratio (OR) = 2.5, 95% confidence interval (CI): 1.2 - 5.3) after adjusting for age, gender, initial ICH volume, and comorbidities (Tables 2, 3).
 Click to view | Table 2. Secondary Outcomes and Functional Impairment at 6 Months |
 Click to view | Table 3. Logistic Regression Analysis |
Of the 11 deaths, 72.7% (eight patients) were due to neurological causes, primarily increased intracranial pressure (45.4%, five patients) from worsening hematoma, brain swelling, and herniation. Recurrent ICH accounted for 18.1% (two patients), and status epilepticus caused 9.1% (one patient). Non-neurological causes accounted for 27.3% (three patients), including sepsis (18.1%, two patients) and acute myocardial infarction (9.1%, one patient) [8, 9].
Results related to hemorrhagic brain topography
The study analyzed hemorrhage locations, distinguishing between lobar and deep subcortical hemorrhages (Fig. 1). Lobar hemorrhages occurred in 32 patients (39%), while deep subcortical hemorrhages were found in 50 patients (61%). Outcomes differed significantly between the two groups [10, 11]. Mortality was higher in lobar hemorrhages, with 21.9% (7/32) of patients dying, compared to 8% (4/50) in the deep subcortical group (P = 0.02). Functional impairment (mRS > 3) was also more frequent in lobar cases, affecting 68.8% (22/32) versus 48% (24/50) of deep subcortical cases (P = 0.04) [10].
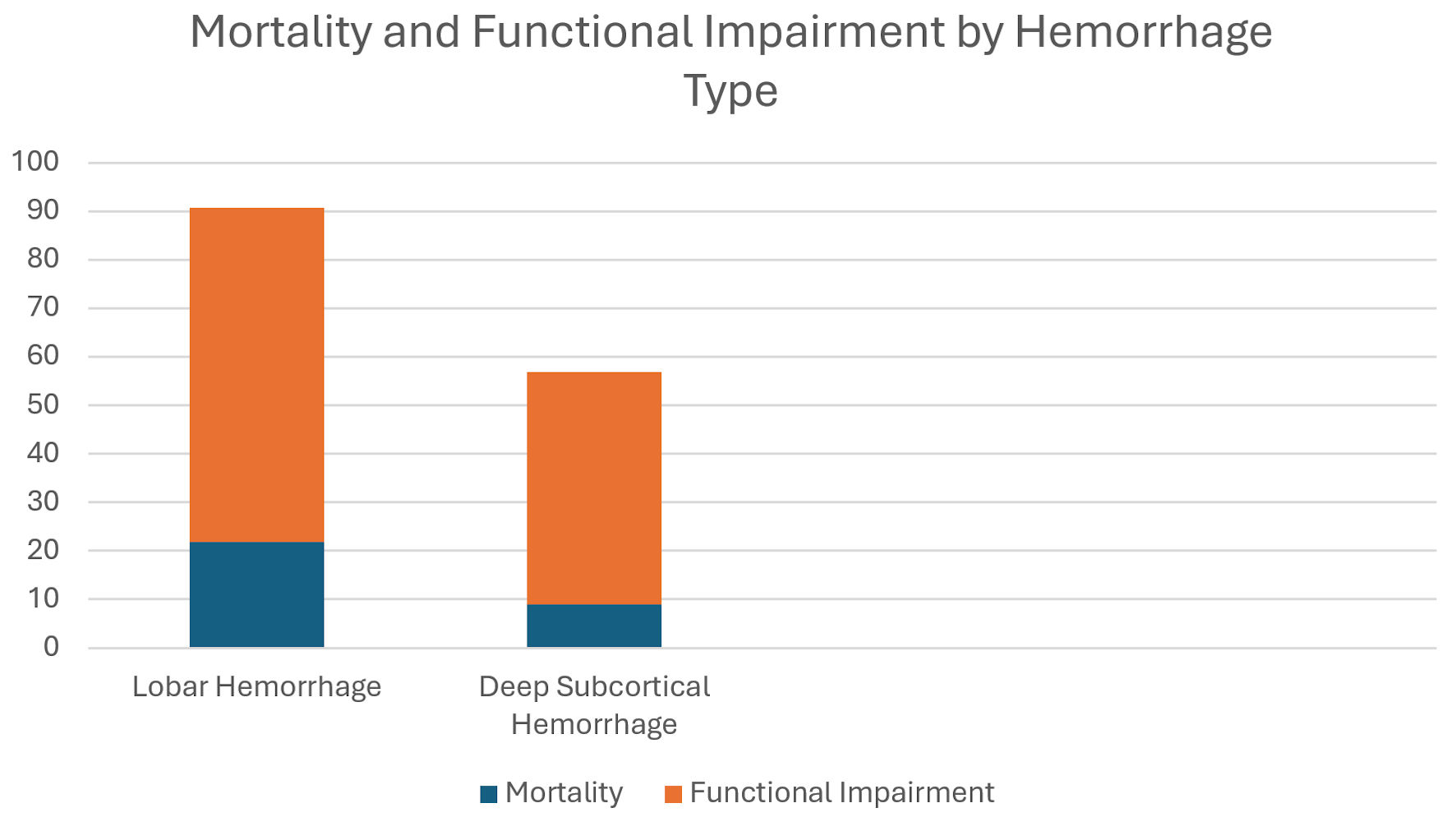 Click for large image | Figure 1. Mortality and functional impairment by hemorrhage type. |
Patients with lobar hemorrhages and elevated ESR had the worst outcomes, suggesting inflammation may exacerbate the negative effects of lobar hemorrhages [12].
Functional impairment
At 6 months, 46 patients (56.1%) had moderate to severe disability (mRS score > 3). The proportion of patients with functional impairment was significantly higher in the elevated ESR group compared to the normal ESR group (65.7% vs. 34%, P = 0.002) [12]. Logistic regression analysis indicated that elevated ESR was independently associated with functional impairment (OR = 3.1, 95% CI: 1.5 - 6.5) after adjusting for potential confounders (Tables 2, 3).
Predictive accuracy of elevated ESR for mortality and functional outcomes
The diagnostic performance of elevated ESR (> 20 mm/h) was assessed for predicting mortality and functional impairment.
For mortality, elevated ESR showed a sensitivity of 63.6% and specificity of 61.8%. While its positive predictive value (PPV) was low at 20%, its negative predictive value (NPV) was high at 91.5%, making normal ESR a strong predictor of survival [10].
For functional impairment (mRS > 3), elevated ESR had a sensitivity of 65.2% and specificity of 70.8%. Its PPV was high at 85.7%, indicating a strong association with disability, but its NPV was lower at 53.2%, making normal ESR less reliable for ruling out disability (Table 2).
Secondary outcomes
Length of hospital stay
Patients with elevated ESR had a longer average hospital stay (mean 18.5 days) compared to those with normal ESR (mean 12.3 days, P = 0.01) (Table 2) [6].
ICH volume
The average ICH volume was higher in patients with elevated ESR (mean 42.6 mL) compared to those with normal ESR (mean 35.2 mL, P = 0.04) (Table 3) [13].
Rehabilitation needs
A greater proportion of patients with elevated ESR required intensive rehabilitation services post-discharge (58.6% vs. 31.9%, P = 0.005) (Table 2) [6].
Inflammatory markers correlation
CRP levels
There was a significant positive correlation between ESR and CRP levels (r = 0.65, P < 0.001), suggesting that higher ESR levels were associated with increased systemic inflammation (Table 4) [14].
 Click to view | Table 4. Correlation with Inflammatory Markers |
Leukocyte count
Elevated ESR was also correlated with higher leukocyte counts (r = 0.53, P < 0.01) (Table 4) [15].
Subgroup analysis
Age groups
In patients aged 70 and above, elevated ESR was an even stronger predictor of mortality (OR = 3.8, 95% CI: 1.7 - 8.3) compared to younger patients (OR = 1.9, 95% CI: 1.0 - 3.6) (Table 5) [7].
 Click to view | Table 5. Subgroup Analysis |
Gender differences
The impact of elevated ESR on functional impairment was more pronounced in male patients (OR = 3.4, 95% CI: 1.7 - 7.0) compared to female patients (OR = 2.2, 95% CI: 1.1 - 4.4) (Table 5) [16].
| Discussion | ▴Top |
This study highlights the significant prognostic value of ESR in patients with ICH. Elevated ESR at admission was independently associated with higher mortality and greater functional impairment at 6 months. These findings suggest that ESR, a readily available and inexpensive test, could be used to identify ICH patients at higher risk of poor outcomes [13].
The relationship between elevated ESR and poor outcomes in ICH may be explained by several mechanisms. Inflammation plays a crucial role in the pathophysiology of ICH, contributing to secondary brain injury [1]. Elevated ESR reflects an inflammatory state, which may exacerbate brain edema, increase intracranial pressure, and promote neurotoxicity, leading to worse outcomes. Additionally, systemic inflammation may impair recovery processes, further contributing to disability and mortality [4, 5, 14, 15].
Previous studies have shown that other inflammatory markers, such as CRP and interleukin-6 (IL-6), are associated with outcomes in stroke patients [14, 15, 17]. Our study extends these findings by demonstrating the prognostic significance of ESR specifically in ICH patients. ESR has advantages over other inflammatory markers due to its widespread availability, low cost, and ease of measurement.
Hematological disorders, though rare, can manifest as acute spontaneous ICH in humans, and their differentiation from other causes of hemorrhagic stroke is critical. Disorders such as coagulopathies, platelet dysfunction, or hematologic malignancies can directly precipitate ICH, particularly in the absence of trauma or other obvious risk factors. This is a key distinction because such conditions demand specific diagnostic and therapeutic strategies compared to hypertensive or amyloid angiopathy-related ICH [18].
Clinical implications
The identification of elevated ESR as a prognostic factor in ICH has important clinical implications. First, it can aid in risk stratification, allowing clinicians to identify patients who may benefit from more intensive monitoring and early interventions. For instance, patients with elevated ESR may require closer neurological observation, more aggressive management of intracranial pressure, and early rehabilitation efforts to optimize functional outcomes [13].
Second, ESR could be incorporated into prognostic models to improve their accuracy and predictive value. Current prognostic models for ICH primarily focus on clinical and radiological factors such as age, ICH volume, and Glasgow Coma Scale score. Adding ESR to these models may enhance their ability to predict outcomes and guide treatment decisions [15, 16].
Accurate identification of hematological disorders as a cause of ICH is critical, as it requires distinct management strategies, such as blood product replacement, reversal of anticoagulation, or disease-specific therapies. These conditions also carry a higher risk of recurrence if left untreated. Routine hematologic screening should be prioritized, particularly in non-hypertensive ICH or atypical cases like lobar hemorrhages in younger patients. Collaboration with hematology specialists is essential when coagulopathies or other systemic hematological disorders are suspected, ensuring appropriate diagnostic workup and treatment to improve patient outcomes [9].
Lastly, our findings underscore the importance of inflammation in the pathophysiology of ICH. Future research should investigate the potential benefits of anti-inflammatory therapies in ICH patients with elevated ESR. Interventions targeting inflammation could mitigate secondary brain injury and improve outcomes.
Future research directions
This study suggests several directions for future research. Large-scale, multicenter, prospective studies are needed to validate ESR’s prognostic value and its integration into risk models for predicting ICH outcomes. Comparative studies of ESR alongside specific inflammatory markers like IL-6, tumor necrosis factor (TNF)-alpha, and fibrinogen could refine our understanding of inflammation in ICH. Experimental research is essential to explore how elevated ESR contributes to secondary brain injury and poor outcomes, while clinical trials on anti-inflammatory therapies may reveal potential treatment benefits. Additionally, future studies should assess how hemorrhage location affects ESR’s prognostic significance, considering the differences in clinical course and pathophysiology between lobar and deep hemorrhages. Long-term follow-up studies are also necessary to evaluate ESR’s role in predicting functional recovery and recurrence of ICH.
Study limitations
This study provides important insights into the prognostic role of ESR in ICH patients; however, several limitations must be acknowledged. First, the retrospective design introduces potential biases, especially concerning variables like the timing of ESR measurement relative to ICH onset, which varied across patients. Additionally, as the study was conducted at a single center, the generalizability of the findings to other populations with different demographics or clinical characteristics may be limited. The relatively small sample size of 82 patients further restricts the statistical power, especially for subgroup analyses, and may limit the ability to detect differences or interactions between variables.
Unmeasured confounders, such as pre-existing inflammatory conditions, or variations in treatment protocols, could have influenced the outcomes, despite adjustments for key variables. While ESR is a useful marker for inflammation, it is nonspecific, and the study did not explore other potentially more specific markers, such as IL-6 or fibrinogen, which could offer additional prognostic value.
Although secondary causes of ICH were excluded, the criteria used to identify non-hypertensive mechanisms might have overlooked subtle or undiagnosed causes, including occult hematological disorders. Finally, with a follow-up period of only 6 months, long-term outcomes such as persistent functional impairment and mortality were not fully captured, which limits the ability to assess the full clinical trajectory of these patients.
Conclusions
In conclusion, this study demonstrates that elevated ESR at admission is an independent predictor of mortality and functional impairment in patients with ICH. ESR, a simple and inexpensive test, provides valuable prognostic information and can aid in risk stratification and clinical decision-making. These findings emphasize the role of inflammation in ICH and highlight the need for further research to explore therapeutic strategies targeting inflammatory pathways.
Further studies are needed to explore the prevalence and outcomes of ICH in patients with underlying hematological disorders. Incorporating advanced diagnostic tools (e.g., genetic testing for clotting disorders) may improve detection and inform treatment paradigms.
Acknowledgments
We would like to express our gratitude to the medical staff at the participating hospitals for their invaluable assistance in collecting patient data and providing care for the study participants. Our sincere thanks to the patients and their families for their cooperation and participation in this study.
Financial Disclosure
This research was not supported by any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None to declare.
Informed Consent
All participants in the study provided informed consent prior to their inclusion.
Author Contributions
Ereida Rraklli: conceptualization of the study, data collection, analysis, and drafting the manuscript. Frenki Gjika: data analysis, interpretation of results, and critical revision of the manuscript. Oneda Cibuku assisted in data collection, literature review, and contributed to manuscript preparation. All authors have reviewed and approved the final version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author, Ereida Rraklli, upon reasonable request.
| References | ▴Top |
- An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke. 2017;19(1):3-10.
doi pubmed - Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759-771.
doi pubmed - Wang S, Zou XL, Wu LX, Zhou HF, Xiao L, Yao T, Zhang Y, et al. Epidemiology of intracerebral hemorrhage: A systematic review and meta-analysis. Front Neurol. 2022;13:915813.
doi pubmed - Menon V, Venu S, Andrade C. Inflammatory markers in acute ischemic stroke with and without preexisting major depression: Methodological issues. Indian J Psychiatry. 2020;62(1):108-109.
doi pubmed - Emsley HC, Tyrrell PJ. Inflammation and infection in clinical stroke. J Cereb Blood Flow Metab. 2002;22(12):1399-1419.
doi pubmed - Flaherty ML, Haverbusch M, Sekar P, Kissela B, Kleindorfer D, Moomaw CJ, Sauerbeck L, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66(8):1182-1186.
doi pubmed - Fest J, Ruiter R, Mooijaart SP, Ikram MA, van Eijck CHJ, Stricker BH. Erythrocyte sedimentation rate as an independent prognostic marker for mortality: a prospective population-based cohort study. J Intern Med. 2019;285(3):341-348.
doi pubmed - Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24(7):987-993.
doi pubmed - Martinez J, Mouzinho M, Teles J, Guilherme P, Nogueira J, Felix C, Ferreira F, et al. Poor intensive stroke care is associated with short-term death after spontaneous intracerebral hemorrhage. Clin Neurol Neurosurg. 2020;191:105696.
doi pubmed - Mendiola JMF, Arboix A, Garcia-Eroles L, Sanchez-Lopez MJ. Acute spontaneous lobar cerebral hemorrhages present a different clinical profile and a more severe early prognosis than deep subcortical intracerebral hemorrhages-a hospital-based stroke registry study. Biomedicines. 2023;11(1):223.
doi pubmed - Caplan LR. Intracerebral haemorrhage. Lancet. 1992;339(8794):656-658.
doi pubmed - Di Napoli M, Godoy DA, Campi V, Masotti L, Smith CJ, Parry Jones AR, Hopkins SJ, et al. C-reactive protein in intracerebral hemorrhage: time course, tissue localization, and prognosis. Neurology. 2012;79(7):690-699.
doi pubmed - Bader ER, Pana TA, Barlas RS, Metcalf AK, Potter JF, Myint PK. Elevated inflammatory biomarkers and poor outcomes in intracerebral hemorrhage. J Neurol. 2022;269(12):6330-6341.
doi pubmed - Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018;9:754.
doi pubmed - Rendevski V, Aleksovski B, Mihajlovska Rendevska A, Hadzi-Petrushev N, Manusheva N, Shuntov B, Gjorgoski I. Inflammatory and oxidative stress markers in intracerebral hemorrhage: Relevance as prognostic markers for quantification of the edema volume. Brain Pathol. 2023;33(2):e13106.
doi pubmed - Wang SS, Bogli SY, Nierobisch N, Wildbolz S, Keller E, Brandi G. Sex-related differences in patients' characteristics, provided care, and outcomes following spontaneous intracerebral hemorrhage. Neurocrit Care. 2022;37(1):111-120.
doi pubmed - Bernstein JE, Savla P, Dong F, Zampella B, Wiginton JGt, Miulli DE, Wacker MR, et al. Inflammatory markers and severity of intracerebral hemorrhage. Cureus. 2018;10(10):e3529.
doi pubmed - Arboix A, Besses C. Cerebrovascular disease as the initial clinical presentation of haematological disorders. Eur Neurol. 1997;37(4):207-211.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.