| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://jnr.elmerpub.com |
Case Report
Volume 15, Number 2, March 2025, pages 87-92
Implementation of Platelet-Rich Plasma in Regeneration of Spinal Nerve Affected by Symptomatic Disc Herniation
Sarvar A. Bebitova, c , Yakutkhan N. Madjidovab, Dilfuza R. Temirovaa
aNeurology Department, Kimyo International University Hospital, Tashkent 100121, Uzbekistan
bNeurology and Pediatric Neurology, Medical Genetics Department, Tashkent Pediatric Medical Institute, Tashkent 100140, Uzbekistan
cCorresponding Author: Sarvar A. Bebitov, Neurology Department, Kimyo International University Hospital, Tashkent 100121, Uzbekistan
Manuscript submitted November 11, 2024, accepted January 22, 2025, published online February 6, 2025
Short title: Effectiveness of PRP in DDD
doi: https://doi.org/10.14740/jnr868
| Abstract | ▴Top |
Degenerative disc disease (DDD) is characterized by autoimmune inflammation and, in some cases, the development of peripheral paresis, sensory impairment, as well as severe pain due to axonal damage of spinal nerve or root because of compression by a disc herniation. In such cases, conservative treatment is not effective. Delaying surgical intervention can lead to irreversible impairment of nerve function. In some cases, patients refuse surgery and will become disabled for the rest of their lives. Here, in our practice, two patients with peripheral monoparesis, sensory disturbances and leg pain due to a disc herniation in VL4-L5 and VL5-S1 segments were saved from surgical intervention after retrodiscal, epidural and infraneural injection of platelet-rich plasma (PRP), even though there was an indication for surgery. Conservative treatment was ineffective in both patients. Although patients, who are candidates for surgery, always undergo surgical intervention, in our case because of PRP injection in proper places, patients were saved from operation. This compels neurosurgeons and physicians, who treat patients traditionally, to think deeply before referring patients to the operation room and increases our knowledge in the treatment plane. There was a decrease in the inflammatory process and recovery of the nerve function over a short period, as well as regression of the symptoms of the disease because of PRP. Hence, injecting PRP into a proper place in complicated herniated disc disease can stimulate nerve regeneration and decrease an inflammation process that can prevent surgical intervention.
Keywords: Degenerative disc disease; Degeneration; Platelet-rich plasma; Growth factors
| Introduction | ▴Top |
Degenerative disc disease (DDD) as an autoimmune inflammatory process leads to the breakdown of extracellular components, which can activate signaling pathways that stimulate to increase an expression of cytokines (interleukin (IL)-1β, tumor necrosis factor (TNF)-α, IL-6, IL-8, IL-17, and interferon (IFN)-γ). Increased levels of cytokines in DDD perpetuate the destruction of disc tissue by increasing the expression of aggrecanases and matrix-degrading proteases and initiate deleterious feedback leading to further expression of inflammatory cytokines in the disc tissue [1-4]. As a result, the production of inflammatory mediators in the degenerated tissue increases and stimulates neoangiogenesis and the formation of new nerve endings, which causes discogenic pain [5-8]. The complexity of pathophysiology and lack of any treatment suspending the degeneration and stimulating the regeneration process lead to the spread of the degeneration process inside the disc. The development of a disc herniation (DH) causes compression of the nerve root, which can lead to peripheral paresis, plegia and severe pain. In such cases, conservative treatment is almost not useful and surgical intervention is required. The absence of blood vessels inside the disc prevents the efficiency of any treatment including intradiscal injections of stem cells, platelet-rich plasma (PRP). Perhaps in the early stages of DDD, the cellular therapy adding bioactive substances will have an opportunity to stop degeneration and, maybe, stimulate some regeneration.
Up to the present day, several scientific works have been carried out related to the introduction of PRP injection inside the disc [9-12], but no one condition has been reported about prevention from operation of DH due to its complications after PRP injection or other cellular therapy. In this case report, two patients with paralyzing sciatica, sensitive impairment and severe pain in their legs due to DH in VL4-L5 and VL5-S1 segments have been reported as being saved from surgery intervention after the retrodiscal, epidural and infraneural injection of PRP.
| Case Report | ▴Top |
Two patients (case 1: 39 years old; case 2: 60 years old) were diagnosed DH with a neurological deficit. The patients had different times of evolution but similar symptoms: sciatica and weakness in the left leg. Owing to the failure of conservative treatment, they were admitted to the hospital. After complementary studies (TNF-α in blood, magnetic resonance imaging (MRI), nerve conduction study (NCS) and needle electromyography (EMG)), surgical intervention was recommended. Both patients refused.
Case 1 suffered from low back pain irradiating to the left leg 10 days ago before admission, while in case 2, similar symptoms started in March 2024. However, case 2 felt weakness in the left leg in June. On the contrary, in case 1, there was paresis in the left leg on the first day of illness and then he started to limp. Both patients were treated conservatively without any effects. After that, they were admitted to our hospital in September. Both patients underwent MRI, NCS of peripheral nerves and EMG examinations. To assess the inflammation process activity, TNF-α was tested in blood. The surgical intervention was approved after examinations, but both patients refused. Therefore, 2 mL PRP was injected in retrodiscal epidural space and perineural area under X-ray and ultrasound guidance. The injection was repeated three times in each patient and was carried out after every 4 days. We could not find any retrodiscal and infraneural PRP injection protocol in DH. However, we performed retrodiscal and infraneural PRP injection under X-ray guidance at the L5-S1 segment and under ultrasound guidance at the L4-L5 segment. After the first injection, some improvements including a decrease in pain and paresis had been achieved. Therefore, we decided to inject the second PRP after 4 days with clinical improvement again. This improvement encouraged us to repeat PRP injection for the third time 4 days after the second one. As the reinjection period was short, to increase the healing process, we decided to inject platelet-poor plasma along the injected needle path while spinal needle was being pulled out. It is a fact that, the nerve tissue regenerates slowly, and in many cases damaged nerve tissue remains paretic if not being decompressed. This fact and patients’ agreement to any procedure apart from surgery compelled us to inject PRP in a short time period. All injection procedures were carried out in surgery room and any side effects and complications were not observed after procedures. Injection areas healed well. The inflammatory parameter (TNF-α), previously high, decreased very quickly and due to the improvement in the patients’ conditions, they were discharged. Pain and paresis regressed, and both patients walked as usual without claudication.
On objective examination, the general condition of both patients was relatively satisfactory, and both patients limped on their weak legs. Skin and visible mucous membranes were clean, with normal color. Peripheral lymph nodes were not enlarged. No deformities were found in the musculoskeletal system. Body mass indexes were normal. Vesicular breathings in the lungs were revealed on auscultation. Heart sounds were clear. Blood pressure was normal. Pulses were rhythmic. The liver and spleen were not enlarged. Defecation and urination were regular.
On neurological status at admission for case 1, cranial nerves were normal. Peripheral monoparesis was found in the left leg. The muscle strengths in the upper extremity and the right leg proximally and distally were 5 points out of 5, whereas 3 points in the proximal muscles and 2 points in the distal muscles were revealed out of 5 in the left leg. Muscle tones were decreased in the left leg. Tendon reflexes: biceps and triceps reflexes were excited equally, whereas patellar and ankle reflexes were weaker on the left. Pathological reflexes were not found. In the sensory sphere, pain sensitivity in the L5 segment of the left leg changed in the form of hypoesthesia. The coordinator system was normal. Meningeal signs were negative. Lasegue I symptom was positive at 30° on the left. The function of the pelvic organs was not impaired. The paravertebral points in the lumbar region were painful. The tone of the paravertebral muscles on the left was increased. Cognition was normal.
For case 2 on admission, cranial nerves were normal. Peripheral, distal monoparesis was found in the left leg. The muscle strengths in the upper extremity and the right leg proximally and distally were 5 points out of 5, whereas 3 points were estimated in the left peroneal group muscles. Muscle tones were hypotonic in the left leg. Tendon reflexes: biceps and triceps reflexes were excited equally, whereas patellar and ankle reflexes were weaker on the left. Pathological reflexes were not found. In the sensory sphere, pain sensitivity in the L5, S1 segments of the left leg changed in the form of hypoesthesia. The coordinator system was normal. Meningeal signs were negative. Symptoms of tension were negative. The function of the pelvic organs was not impaired. The paravertebral points in the lumbar region were painful. The tone of the paravertebral muscles on the left was slightly increased. Cognition was normal.
In a biochemical blood test, the levels of TNF-α were elevated among inflammatory mediators. On admission, TNF-α for case 1 was 17.3 pg/mL (normal level limit 2.5 pg/mL), whereas for case 2, it was 23.7 pg/mL. Other laboratory examinations were normal. On MRI, in case 1, subarticular and foraminal DH on the left with spinal ganglion bulging in the L4-L5 segment was observed as a primary cause of leg pain and weakness (Fig. 1). The MRI of case 2 showed herniated disc lateralizing to the left in the L5-S1 segment (Fig. 2). NCS found an axonal damage in both patients, while needle EMG found a mild increase of amplitude of motor unit action potential (MUAP) in paretic muscle in case 2 and reinnervation-denervation process with spontaneous activities like fibrillation potential and positive sharp wave in case 1 (Supplementary Materials 1, 2, jnr.elmerpub.com). Both patients refused surgical intervention, so they were prescribed standard treatments according to the recommendations of the Ministry of Health of the Republic of Uzbekistan. Both patients were prescribed tenoxicam 20 mg intravenous, tolperisone hydrochloride 150 mg twice orally, dexamethasone 8 mg intravenous, vitamin B complex intramuscular, L-lysine aescinat 10 mL intravenous, and betamethasone + vitamin B12 + diclofenac 3 mL.
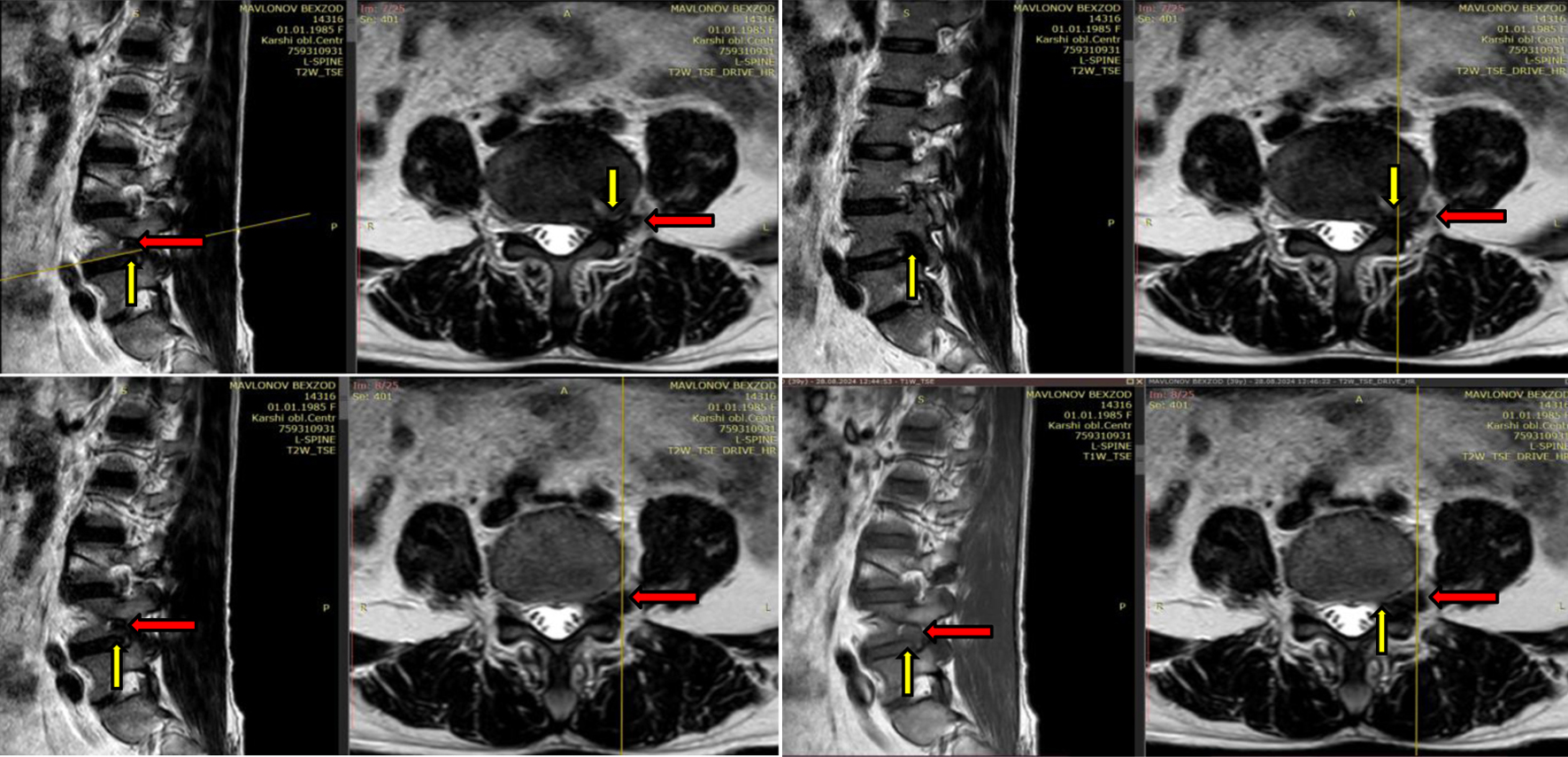 Click for large image | Figure 1. MRI examination of case 1. Degeneration of the discs, Pfirrmann grade IV at L3-L4, L4-L5 levels with foraminal disc herniation (yellow arrow) at L4-L5 level on the left and L4 spinal nerve’s ganglion bulging (red arrow) due to inflammation. Subarticular stenosis. MRI: magnetic resonance imaging. |
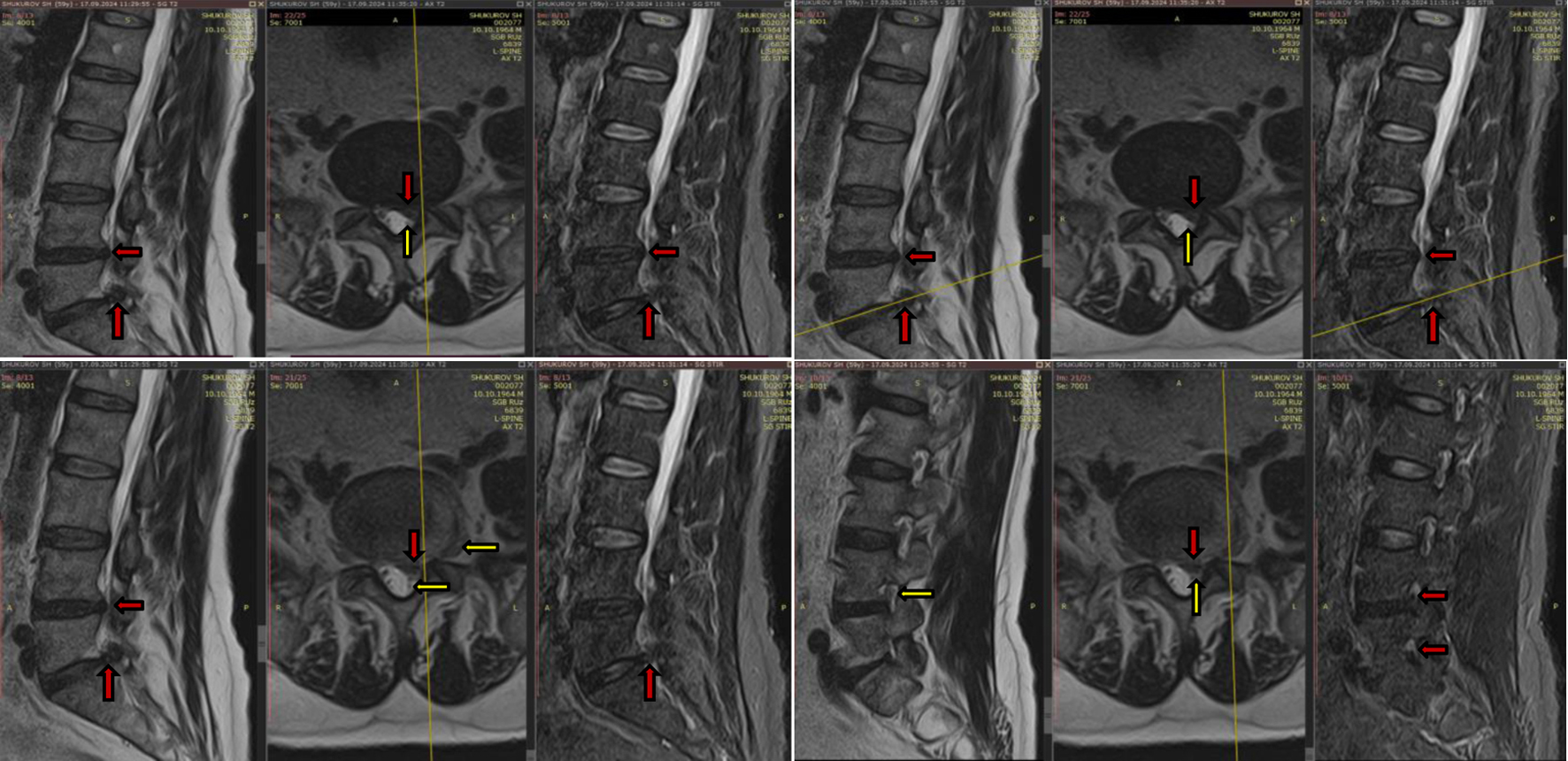 Click for large image | Figure 2. MRI examination of case 2. Degeneration of the discs, Pfirrmann grade IV at L4-L5 (3.6 mm), L5-S1 (8 mm) levels with disc herniation (red arrow). L5-S1 herniated disc injured L5, S1 spinal nerves (yellow arrow) on the left. Secondary stenosis of the spinal canal. MRI: magnetic resonance imaging. |
Five days after the start of treatment, in our hospital, some decrease in the pain was observed in both patients. However, patients were not satisfied. Additionally, paresis remained. Both patients were previously treated conservatively. Case 1 was prescribed dexketoprofen 2 mL intramuscular for 10 days, vitamin B complex intramuscular for 10 days, L-lysine aescinat 10 mL intravenous for 5 days, tolperisone hydrochloride 150 mg twice orally for 10 days, omeprazole 20 mg orally, betamethasone + vitamin B12 + diclofenac 3 mL for 5 days and physiotherapy (laser, magnet therapy, amplipulse therapy with analgesics and non-steroidal anti-inflammatory drug (NSAID)). Case 2 also got the same group of medicines, but three times with a period of 2 - 3 weeks rest. In addition to the medicines, he took rehabilitating physical exercises for 3 months. After that, some decrease of pain had been observed, but not fully disappeared, and paresis remained. Conservative treatment was not fully effective; therefore, patients received 2 mL of epidural, retrodiscal and subneural PRP injections three times every 4 days at the L4-L5 level under ultrasound guidance for case 1 and at the L5-S1 level under X-ray guidance for case 2 (Fig. 3). To prepare PRP, in the operating room of the surgical department, 13.5 mL blood was taken from the patient’s venous blood under sterile conditions using a 20 mL syringe containing 1.5 mL of sodium citrate anticoagulant. The mixture of blood and anticoagulant was poured into a special YCELLBIO-KIT tube at an angle of 45°, after which 2 mL of PRP and 4 mL of platelet-poor plasma were obtained using an angular centrifuge with a frequency of 3,600 Hz after rotation for 6 min. PRP injection was repeated three times in both patients, and every injection was carried out after every 4 days. After PRP injection course, TNF-α decreased almost three times, to 5.6 pg/mL in case 1 and to 7.8 pg/mL in case 2 within 7 days. After the full course of PRP therapy, there was an improvement in neurological status with increased muscle power in both patients. The power of muscle strength in case 1 set up to 5 points proximally and 4 points distally, whereas in case 2, distal group muscle power reached 4 points out of 5. Claudication on the left leg disappeared in both patients. Due to the improvement in patients’ conditions, they were discharged.
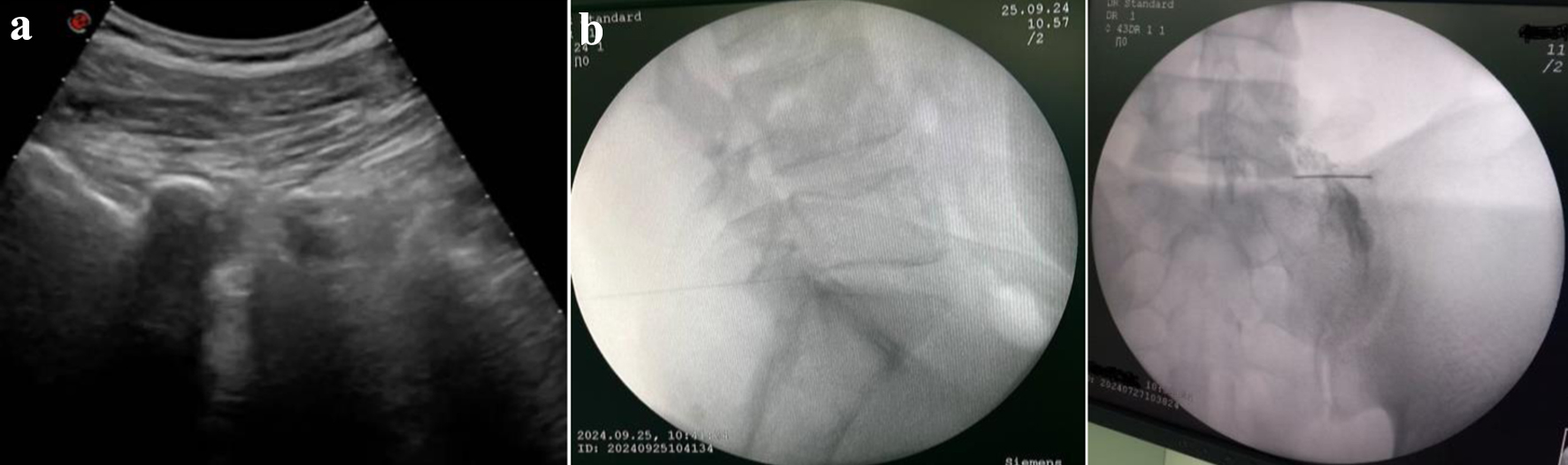 Click for large image | Figure 3. (a) Ultrasound-guided foraminal injection at L4-L5 level. (b) Fluoroscopy-guided epidural retrodiscal injection at L5-S1 level. |
Several scales were used, in particular, the visual analogue scale (VAS) for pain assessment, the modified MacNab scale (mMacNub) for assessing the effectiveness of the treatment, the Oswestry low back disability index (ODI) for assessing the ability to work, and the Nurick scale for assessing the functional state of the patients before and after treatment (Table 1). The results were taken on admission and after 14 days of treatment.
 Click to view | Table 1. Results of Treatment Effectiveness According to Scales |
From Table 1, it is clear that, according to the VAS, the pain disappeared in case 1, while for case 2, a dramatic decrease in pain could be seen. According to the ODI, the disability of both patients disappeared and returned to a mild disability. The patients started to carry out daily routines independently and perform tasks in social life. As for the Nurick scale, only mild radicular symptoms remained for a short period.
Both patients were recommended swimming, kinesitherapy and exercise therapy. However, only case 2 has been taking exercise therapy. As for case 1, he did not follow our recommendation, because as he is a military man, he could not. Nevertheless, case 1 does not feel any pain and discomfort, even paresis has recovered fully after 3 months. After 3 months, case 2 announced that he feels mild pain and tingling after long standing and walking more than 1 km.
As restored parameters can be seen after 1 month in EMG and NCS after clinical improvement, we did not approve repeating the electrodiagnostic tests in both patients. Both patients were recommended to repeat NCS and EMG after 1 - 2 months and MRI after 3 months.
| Discussion | ▴Top |
In experiments conducted to date, it has been proven that PRP containing growth factors including transforming growth factor-β (TGF-β), platelet-derived growth factor (PDGF), epidermal growth factor (EGF), vascular endothelial growth factor (VEGF) and insulin-like growth factor (IGF) inhibits degeneration in the nucleus pulposus (NP) of the disc, improves cell viability and extracellular matrix metabolism, stimulates proliferation of intervertebral disc cells [6] and has an anti-inflammatory effect by influencing cytokines and metalloproteinases [2]. In addition, the analgesic effect of PRP in degenerated tissues has been proven, but this effect does not last long [9]. However, PRP has not been used in combination with conservative treatment until now. Additionally, the use of PRP in DH with neurological deficit is completely unusual and must be understood as “the last chance” in these two patients. Nevertheless, we found improvement in subjective symptoms (VAS, MacNub and ODI scales) and objective (TNF and EMG) parameters. In the clinical case from our practice, the introduction of retrodiscal, epidural and subneural PRP injection was used in patients with DH which led to peripheral paresis due to the spinal nerve damage. In our practice, PRP helps to reduce autoimmune inflammation by decreasing indicators of inflammation mediators in a short time. Meanwhile, PRP stimulated the regeneration of the spinal nerves due to which the function of spinal nerves set up and paresis disappeared. According to the VAS, mMacNub, ODI and Nurik scales, good results were also achieved. Despite the indication for surgical intervention due to the presence of severe lower back pain, the pain in the left leg, monoparesis, and axonal damage on NCS as well as needle EMG, after the procedure, the symptoms quickly regressed and no surgical intervention was required. Typically, after axonal damage, a denervation process and spontaneous activities like fibrillation, pathological sharp wave, as well as fasciculations are detected, which can be seen in the needle EMG for case 1. However, denervation process on needle EMG usually disappears after 2 - 3 months and after that period, needle EMG reveals either full reinnervation or denervation. In case 2, we have faced with this condition. Accordingly, depending on the reinnervation process and over time, the parameters of the MUAP change and polyphasia appears, the amplitude and duration increase, and a satellite may also appear. The sprouting mechanism is activated and the reinnervation process begins (if the ability to regenerate is maintained) on account of healthy nerve root or not fully dead axons in the damaged spinal nerve. The denervation process slows down if the damaged nerve root is not decompressed. When the reinnervation process is completed, muscle function is completely restored. However, it should be taken into account that usually, when a nerve fiber or motor neuron is damaged, only after a certain period, the signs of denervation have developed on the needle EMG in the muscles innervated by this motor neuron or axon. This period depends on the distance. For example, when a nerve root is damaged, the first sign of the denervation process on the needle EMG is determined in the adjacent paravertebral muscles after 10 - 14 days, in the proximal muscles after 2 - 3 weeks, in the distal muscle group after 3 - 4 weeks, and in more distal muscles after 5 - 6 weeks. Therefore, pathological spontaneous activities like positive sharp wave and fasciculation were revealed in needle EMG in case 1, while in case 2, spontaneous activities were not observed because of long time after the spinal nerve damage. In both patients with acute and subacute spinal nerve impairment due to DH, retrodiscal and subneural injection of PRP stimulated the regeneration of the nerve tissue and accelerated the reinnervation process, in which muscle power increased and nerve function improved. Additionally, the inflammation has been decreased. The levels of TNF-α decreased to normal at 1.78 and 2.3 ng/mL in cases 1 and 2, respectively. It is also a fact that the function of acute damaged spinal nerve revived fully and faster, while damaged spinal nerve after a while has not fully recovered. However, in case 2, regeneration process could also be seen after PRP injection. Thus, in both conditions, patients were prevented from surgical intervention due to PRP.
Conclusion
In conclusion, this atypical treatment must be kept in mind when “the standard” has failed. On the other hand, this paper collects a lot of data and analyzes them before and after PRP injection, showing its effect on decreasing inflammation and accelerating the restoration of damaged nerve tissue.
| Supplementary Material | ▴Top |
Suppl 1. NCS and needle EMG results of case 1. During NCS on the nerves of the legs along the tibial and peroneal nerves, there is an asymmetry in amplitude along the tibial nerve on the left by more than 40%, but the parameters are within normal limits for motor responses, symmetrical, reference values. For sensory responses, the parameters are normal, symmetrical. According to needle EMG, in the anterior and posterior tibial muscles, the MUAPs are increased in amplitude and duration by 20% of normal; in the abductor muscle of the thigh (L5 segment), there is a moderate increase in amplitude with normal duration of the MUAPs; spontaneous activities like positive sharp wave and fasciculation in the anterior and posterior tibial muscles on the left are a sign of an active neural reinnervation-denervation process at the L4-5 level on the left (root); the process is active and acute. EMG: electromyography; NCS: nerve conduction study.
Suppl 2. NCS and needle EMG results of case 2. During NCS on the nerves of the legs along the tibial and peroneal nerves, there were not any anomalies on motor and sensory parts. According to needle EMG, in the posterior tibial muscle, an increased amplitude of MUAPs was found on the left, while other muscles were normal. Spontaneous activities were not observed. Mildly radicular process could be seen on the left. EMG: electromyography; NCS: nerve conduction study.
Acknowledgments
We thank the volunteers who participated in this study, as well as staff at Kimyo International University Hospital for administrative support and for enrolling the study participants. Dr. Ubaydullaeva S.F. is thanked for conducting electrodiagnostic examination and evaluating the assessment of damaged nerve function in the feature beforehand. We also appreciate the staff of the laboratory and the technical assistance of fluoroscopic guidance. The responsibility for the content and any remaining errors, omissions, and inaccuracies is our own. No funding source was involved in the design or conduct of the research or preparation of the manuscript, and the analyses and opinions expressed are those of the authors alone.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
Main author Dr. Sarvar A. Bebitov carried out retrodiscal, epideural and infraneural PRP injection under X-ray as well as ultrasound guidance to both patients. In addition to this, he was responsible for the medical report of case 2 as a main physician and did the literacy search while Dr. Dilfuza R. Temirova was technical assistance during X-ray and ultrasound guidance and helped to prepare PRP. Additionally, she presided the documents of case 1. The manuscript was written by Dr. Sarvar Bebitov. Professor Yakutkhan N. Madjidova is supervisor and controlled the job as well as contributed to the study design.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
DDD: degenerative disc disease; EGF: epidermal growth factor; EMG: electromyography; IFN: interferon; IGF: insulin-like growth factor; IL: interleukin; MRI: magnetic resonance imaging; MUAP: motor unit action potential; NCS: nerve conduction study; NP: nucleus pulposus; ODI: Oswestry disability index; PDGF: platelet-derived growth factor; PRP: platelet-rich plasma; TGF-β: transforming growth factor-β; TNF: tumor necrosis factor; VAS: visual analogue scale; VEGF: vascular endothelial growth factor
| References | ▴Top |
- Akeda K, An HS, Pichika R, Attawia M, Thonar EJ, Lenz ME, Uchida A, et al. Platelet-rich plasma (PRP) stimulates the extracellular matrix metabolism of porcine nucleus pulposus and anulus fibrosus cells cultured in alginate beads. Spine (Phila Pa 1976). 2006;31(9):959-966.
doi pubmed - Kim HJ, Yeom JS, Koh YG, Yeo JE, Kang KT, Kang YM, Chang BS, et al. Anti-inflammatory effect of platelet-rich plasma on nucleus pulposus cells with response of TNF-alpha and IL-1. J Orthop Res. 2014;32(4):551-556.
doi pubmed - Peng B, Hao J, Hou S, Wu W, Jiang D, Fu X, Yang Y. Possible pathogenesis of painful intervertebral disc degeneration. Spine (Phila Pa 1976). 2006;31(5):560-566.
doi pubmed - Weiler C, Nerlich AG, Zipperer J, Bachmeier BE, Boos N. 2002 SSE Award Competition in Basic Science: expression of major matrix metalloproteinases is associated with intervertebral disc degradation and resorption. Eur Spine J. 2002;11(4):308-320.
doi pubmed - Chen WH, Liu HY, Lo WC, Wu SC, Chi CH, Chang HY, Hsiao SH, et al. Intervertebral disc regeneration in an ex vivo culture system using mesenchymal stem cells and platelet-rich plasma. Biomaterials. 2009;30(29):5523-5533.
doi pubmed - Gruber HE, Norton HJ, Hanley EN, Jr. Anti-apoptotic effects of IGF-1 and PDGF on human intervertebral disc cells in vitro. Spine (Phila Pa 1976). 2000;25(17):2153-2157.
doi pubmed - Feng H, Danfelter M, Stromqvist B, Heinegard D. Extracellular matrix in disc degeneration. J Bone Joint Surg Am . 2006;88(uppl 2):25-29.
- Freemont AJ, Watkins A, Le Maitre C, Baird P, Jeziorska M, Knight MT, Ross ER, et al. Nerve growth factor expression and innervation of the painful intervertebral disc. J Pathol. 2002;197(3):286-292.
doi pubmed - Akeda K, Imanisha T, Ohishi K, et al. Intradiscal injection of autologous platelet-rich-plasma for the treatment of lumbar disc degeneration preliminary prospective clinical trial for discogenic low back pain patients. Poster no. 2194 presented at ORS Annual Meeting. 2012.
- Nagae M, Ikeda T, Mikami Y, Hase H, Ozawa H, Matsuda K, Sakamoto H, et al. Intervertebral disc regeneration using platelet-rich plasma and biodegradable gelatin hydrogel microspheres. Tissue Eng. 2007;13(1):147-158.
doi pubmed - Sawamura K, Ikeda T, Nagae M, Okamoto S, Mikami Y, Hase H, Ikoma K, et al. Characterization of in vivo effects of platelet-rich plasma and biodegradable gelatin hydrogel microspheres on degenerated intervertebral discs. Tissue Eng Part A. 2009;15(12):3719-3727.
doi pubmed - Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, et al. Lumbar intradiskal platelet-rich plasma (PRP) injections: a prospective, double-blind, randomized controlled study. PM R. 2016;8(1):1-10; quiz 10.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.