| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://jnr.elmerpub.com |
Case Report
Volume 15, Number 2, March 2025, pages 93-103
Mechanical Thrombectomy During Coiling of Acutely Ruptured Cerebral Aneurysms
Mostafa Mahmouda, e, Osman Koca, Ehab Mahmouda, Ali Ayyadb, Suhail Hussainc, Ahmad Muhammadc, Hassan Haroonc, Yahia Imamc, Ahmed Ownd
aInterventional Neuroradiology Division, Neuroradiology Department, Neuroscience Institute, Hamad General Hospital, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
bMicrovascular Surgery Division, Neurosurgery Department, Neuroscience Institute, Hamad General Hospital, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
cStrokology Division, Neurology Department, Neuroscience Institute, Hamad General Hospital, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
dDiagnostic Neuroimaging Division, Neuroradiology Department, Neuroscience Institute, Hamad General Hospital, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
eCorresponding Author: Mostafa Mahmoud, Interventional Neuroradiology Division, Neuroradiology Department, Neuroscience Institute, Hamad General Hospital, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
Manuscript submitted December 16, 2024, accepted February 3, 2025, published online February 11, 2025
Short title: Mechanical Thrombectomy in Cerebral Aneurysms
doi: https://doi.org/10.14740/jnr872
| Abstract | ▴Top |
Thromboembolic events are common complications encountered during the endovascular treatment of acutely ruptured cerebral aneurysms. Major arterial occlusion may lead to serious neurological consequences, including significant morbidity or even death. While intra-arterial injection of thrombolytic or fibrinolytic agents can be effective for distal thrombus lysis, major arterial occlusion is sometimes resistant to such treatments. This study is a retrospective case series based on our database covering the period from January 2014 to December 2023. Five patients with complete large arterial occlusions occurring during the endovascular treatment of acutely ruptured aneurysms were treated with stent retrievers or direct aspiration. Patients’ demographics, angiographic findings, and clinical outcomes are discussed. A review of the relevant literature in English was also conducted. All occluded arteries were fully recanalized, with no infarctions detected on 24-h follow-up computed tomography scans. One patient, with a grade V on the Hunt and Hess (H&H) scale, died as a result of the disease course. The remaining patients recovered to their pre-intervention neurological baseline. Mechanical thrombectomy during the treatment of acutely ruptured aneurysms allows for rapid recanalization of occluded arteries without the need for intra-arterial thrombolytic or fibrinolytic therapy, yielding favorable clinical outcomes. To the best of our knowledge, this is the first literature review focused on thrombectomy in the context of acutely ruptured aneurysms.
Keywords: Aneurysms; Thrombectomy; Stent retriever; Aspiration; Stroke; Subarachnoid hemorrhage; Coiling
| Introduction | ▴Top |
Thromboembolic complications that occur during endovascular treatment of cerebral aneurysms can lead to significant neurological consequences, with reported incidence rates ranging from 2% to 28% [1-3]. The estimated permanent neurological morbidity ranges from 1.7% to 5% [4, 5], and the mortality rate is approximately 1.9% [6]. Recanalization is critical to prevent devastating neurological outcomes; however, documented cases of arterial occlusion treated with mechanical thrombectomy during the endovascular management of acutely ruptured aneurysms remain limited. This study presents five cases of ruptured aneurysms associated with major arterial occlusion during endovascular treatment, managed using stent retriever or direct aspiration techniques. In addition, a review of the English-language literature was conducted. To the best of our knowledge, this is the first literature review focused on thrombectomy during the treatment of acutely ruptured aneurysms.
From January 2014 to December 2023, 547 patients with ruptured aneurysms underwent coiling, of whom 49 developed thromboembolic complications. Among these, 11 patients experienced large arterial occlusion either intra-procedurally or post-procedurally. Six patients were treated with rescue stenting, while five underwent mechanical thrombectomy. This retrospective study was approved by the ethics board (approval number ID MRC-04-24-080), and informed written consent was obtained from the patients or their first-degree relatives. We confirm that this series does not contain any information that could identify individual patients. Patient data, including demographics, devices used, and outcomes, are summarized in Table 1.
 Click to view | Table 1. Patients Demographics and Clinical Outcome |
| Case Reports | ▴Top |
Technique
All procedures were performed under general anesthesia and systemic heparinization, initiated by administering 5,000 IU of intravenous (IV) heparin once the arterial introducer was in place, followed by 1,000 IU of heparin every hour to maintain an activated clotting time (ACT) between 200 and 250 s. In cases 2 and 5, the artery was catheterized using a Tempo 5 French catheter (Cordis, FL, USA), then an exchange maneuver was performed with a Terumo 0.035 wire, 260 cm in length (Terumo, Japan), to advance the guiding catheter due to challenging arterial tortuosity. A Guider soft tip 8F, 90 cm in length (Boston Scientific, Marlborough, MA), was used in three cases, a Benchmark 7F (Penumbra, Alameda, CA) in one case, and a Neuron Max 6F, 90 cm in length (Penumbra, Alameda, CA), in one case.
Rotational angiography and 3D reconstruction were performed to determine the optimal working projection and accurately measure the aneurysm dimensions. The aneurysms were accessed using an SL-10 microcatheter (Stryker Neurovascular, Fremont, CA) in conjunction with a Synchro 0.014 microwire (Stryker Neurovascular, Fremont, CA). Target coils (Stryker Neurovascular, Fremont, CA) were deployed in all cases under the protection of the balloon remodeling technique. A Hyperglide 4 × 10 mm balloon (Medtronic, Minneapolis, MN) was used in three cases, and a Transform 4 × 10 mm balloon (Stryker, USA) was used in two cases.
In cases where flow arrest occurred in the involved artery, an additional 3,000 IU of IV heparin was administered, followed by navigation of a Rebar 18 microcatheter with a Synchro 0.014 microwire distal to the thrombus. A Solitaire AB 4 × 20 mm thrombectomy device (Medtronic, Minneapolis, MN) was deployed at the occlusion site and slowly retrieved under continuous suction from a guiding catheter connected to a Vaclok syringe (Merit Medical, Utah, USA). Full recanalization, defined as thrombolysis in cerebral infarction (TICI) 3, was achieved in all cases, as assessed by the TICI scale. A follow-up computed tomography (CT) was performed the following day in all cases, revealing no infarctions.
Case 1
A 58-year-old man with a history of hypertension and type 2 diabetes mellitus (T2DM) presented with a Glasgow coma scale (GCS) 4, necessitating rapid intubation. On examination, his pupils were 2 mm, sluggish, and reactive. Non-contrast CT (NCCT) of the head revealed a diffuse subarachnoid hemorrhage (SAH) with no significant ventricular dilation. CT angiography of the head, followed by conventional angiography, revealed a basilar tip aneurysm measuring 7.8 mm in length and 6.1 mm in transverse diameter. After successful aneurysm coiling, left posterior cerebral artery (PCA) occlusion was observed. Therefore, a RED 62 aspiration catheter (Penumbra, Alameda, CA) was advanced to the occlusion site, and subsequent thrombus aspiration resulted in full recanalization (TICI 3) of the left PCA. However, a small clot fragment migrated to the right PCA, causing its occlusion. Another pass using the RED 62 aspiration catheter resulted in full revascularization (TICI 3) of the right PCA (Fig. 1a-d). The ACT at the time of occlusion was 162 s, and 38 min were required for full recanalization. Follow-up CT revealed no infarctions; however, the patient died 48 h later due to the sequelae of the high-grade SAH.
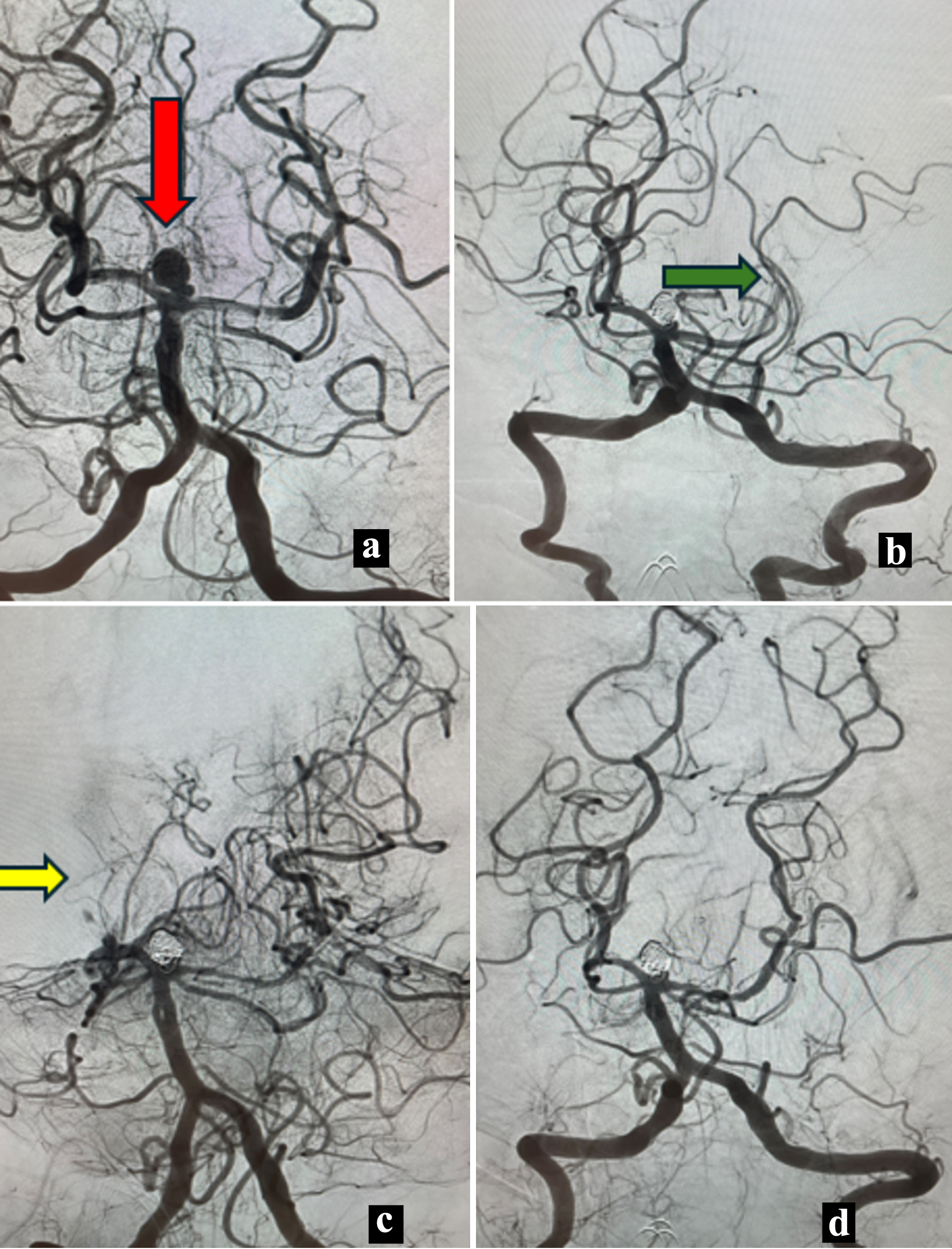 Click for large image | Figure 1. Case 1. (a) Anteroposterior (AP) angiography showing a basilar tip aneurysm (red arrow). (b) AP view with caudal angulation view showing occluded left posterior cerebral artery (PCA) (green arrow). (c) Oblique view angiography showing occlusion of the right PCA (yellow arrow) with patent left PCA. (d) Post mechanical thrombectomy final angiography showing both patent PCAs. |
Case 2
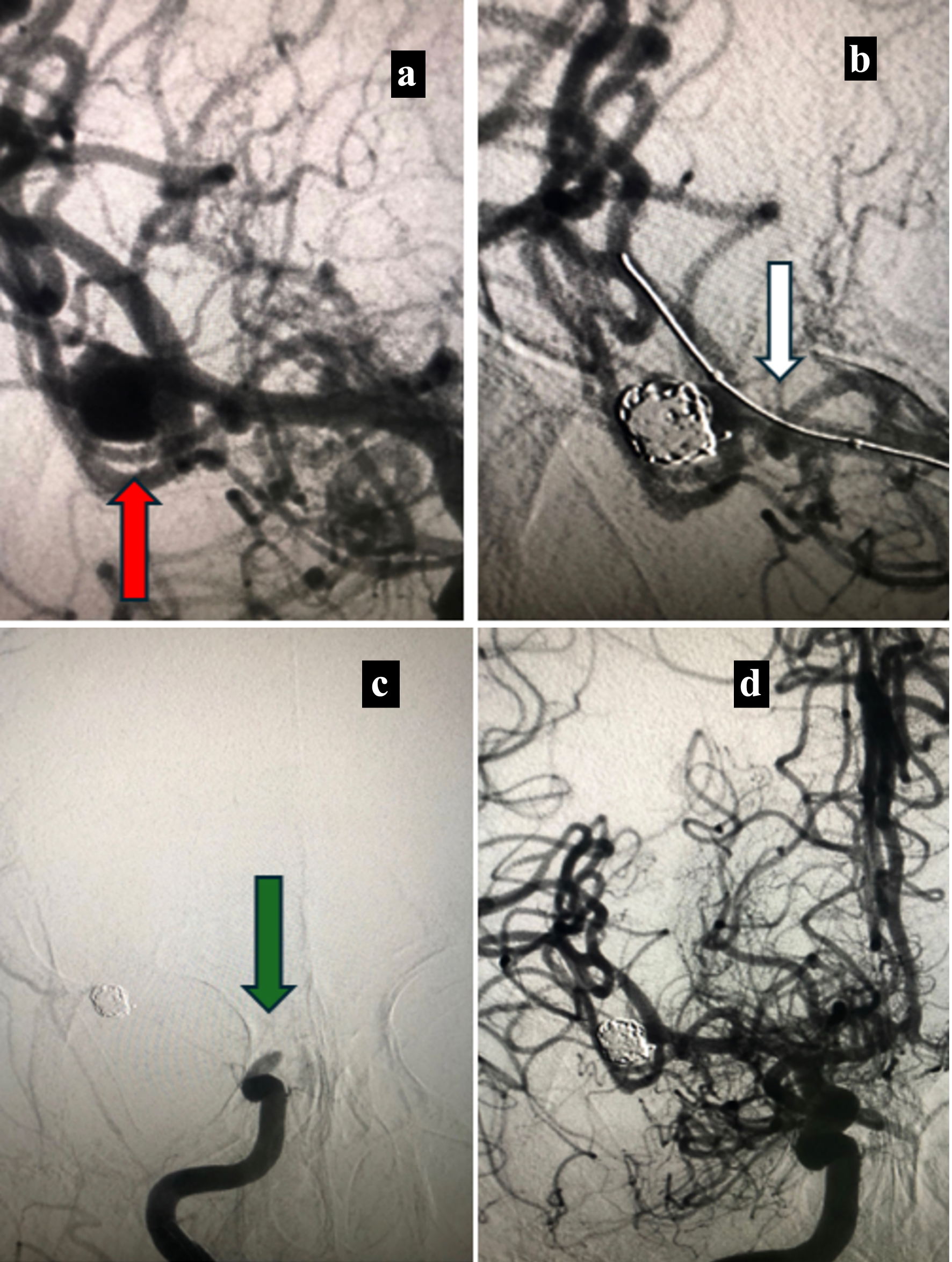
A 50-year-old woman with no significant past medical history presented with a headache and mild nuchal rigidity. On examination, she was fully conscious and oriented, with no ptosis, and her pupils were 2 mm and reactive, and had no motor deficits. NCCT of the head showed a diffuse SAH with right sylvian fissure predominance and no hydrocephalic changes. Conventional angiography revealed a right posterior communicating (PCOM) aneurysm measuring 7 × 6 mm. Following an exchange maneuver to place a guiding catheter, complete occlusion of the M1 segment of middle cerebral artery (MCA) was observed. Full revascularization (TICI 3) was achieved using a Solitaire AB 4 × 20 mm thrombectomy device (Fig. 2a-d). The ACT at the time of occlusion was not measured, and 18 min were required to fully recanalize the MCA. She was discharged home without neurological deficits, with a modified Rankin scale (mRS) score of 0.
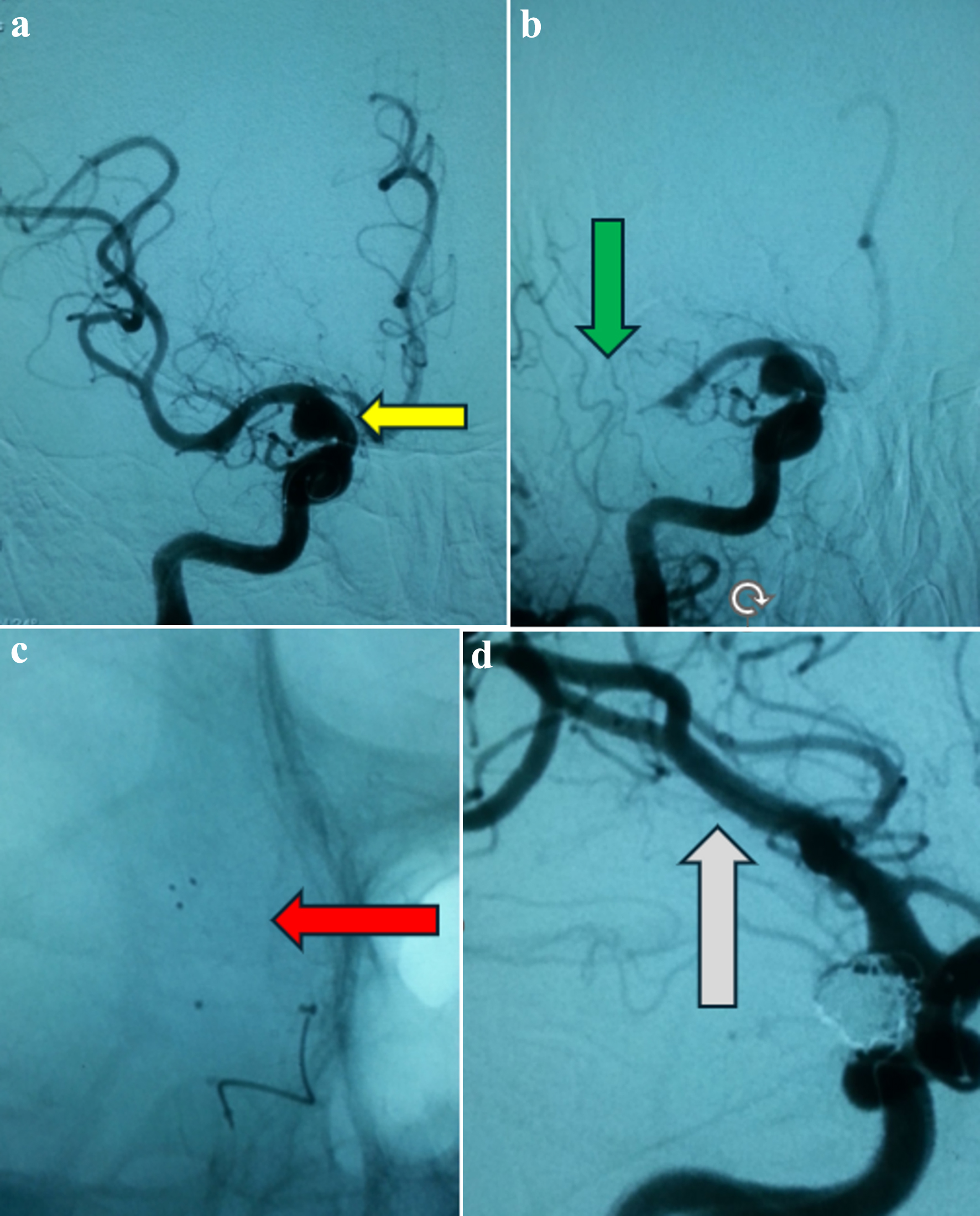 Click for large image | Figure 2. Case 2. (a) Anteroposterior angiographic view showing a posterior communicating aneurysm (yellow arrow). (b) Anteroposterior angiographic view showing occluded M1 segment (green arrow). (c) Native view showing the deployed stent retriever (red arrow). (d) Oblique angiographic view showing the coiled aneurysm with patency of the middle cerebral artery (white arrow). |
Case 3
A 45-year-old man with no significant medical history presented with severe headache, nausea, vomiting, nuchal rigidity, and photophobia. On examination, he was alert and oriented, with no motor deficits. NCCT of the head showed an SAH with interhemispheric predominance. CT angiography of the head and conventional angiography revealed an anterior communicating (ACOM) aneurysm measuring 3 mm in length and 2.5 mm in transverse diameter. Following successful coiling, complete flow arrest was observed at the A1 segment of anterior cerebral artery (ACA) on final control angiography. The thrombus was successfully retrieved in a single pass using a Solitaire AB 4 × 20 mm thrombectomy device, achieving TICI 3 recanalization (Fig. 3a-e). The procedure time from groin puncture to thrombus formation was 42 min, with an ACT of 154 s at the time of thrombus development; 20 min were required for recanalization of the occluded ACA. He was discharged without neurological deficits, with an mRS score of 0.
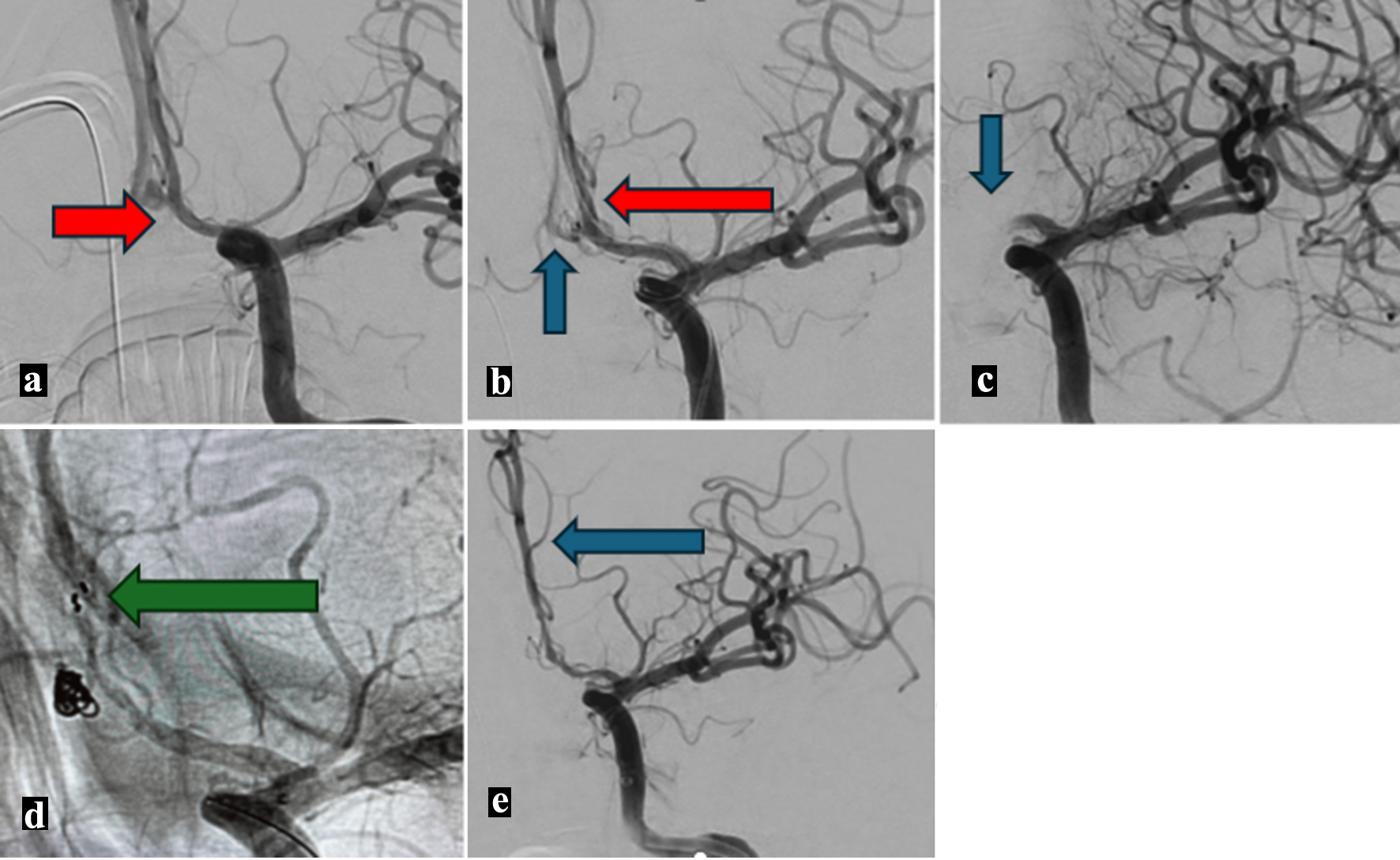 Click for large image | Figure 3. Case 3. (a) Anteroposterior angiography showing an anterior communicating aneurysm (red arrow). (b) Anteroposterior angiography showing the coiled aneurysm (blue arrow) with a remodeling balloon (red arrow). (c) Post coiling anteroposterior angiography showing occluded A1 segment (blue arrow). (d) Anteroposterior native angiography showing patent anterior cerebral artery through the deployed stent retriever struts (green arrow). (e) Final anteroposterior angiography showing patent anterior cerebral artery (blue arrow). |
Case 4
A 36-year-old woman with no significant medical history presented with a mild headache, as well as back and neck pain. NCCT of the head revealed a diffuse SAH. Conventional angiography identified a 7 × 4.6 mm left internal carotid artery (ICA) terminus aneurysm. After deploying the final coil, occlusion of the distal M1 segment of MCA was noted. The microcatheter and balloon were withdrawn, and a Rebar 18 (Medtronic, Minneapolis, MN) was advanced to the MCA. A Solitaire AB stent retriever (4 × 20 mm) was deployed, successfully retrieving the thrombus on the first pass and achieving full recanalization as TICI 3 (Fig. 4a-e). The ACT at the time of occlusion was 154 s, and it took 28 min to restore blood flow. The patient was discharged with no neurological deficits and an mRS score of 0.
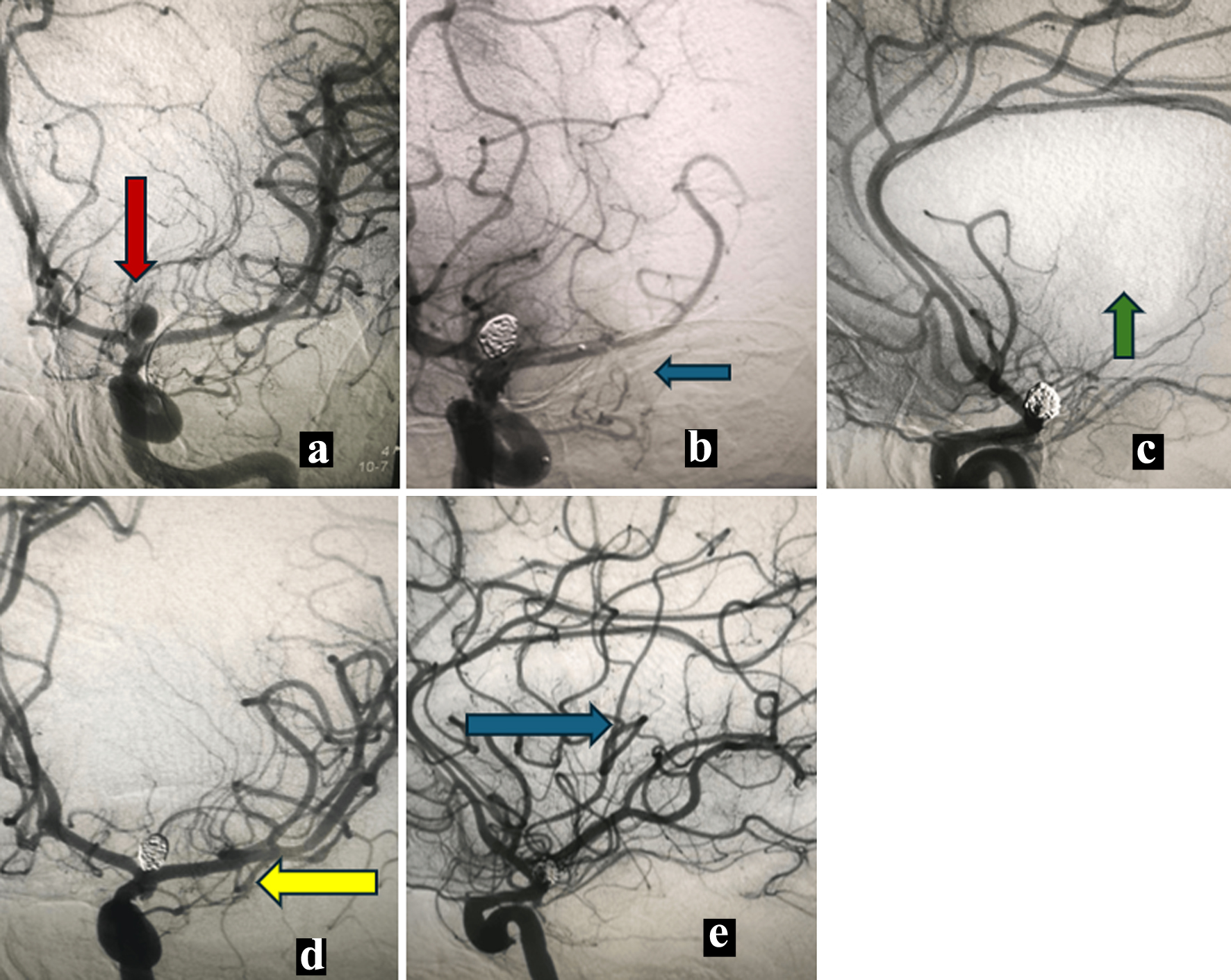 Click for large image | Figure 4. Case 4. (a) Anteroposterior angiography showing internal carotid terminus aneurysm (red arrow). (b) Post coiling of the aneurysm anteroposterior angiography showing M1 occlusion (blue arrow). (c) Lateral view angiography showing occluded middle cerebral artery (green arrow). (d) Post mechanical thrombectomy anteroposterior angiography showing recanalized middle cerebral artery (yellow arrow). (e) Post mechanical thrombectomy lateral view angiography showing recanalized middle cerebral artery (blue arrow). |
Case 5
A 68-year-old woman with a history of hypertension and T2DM presented with a severe headache, confusion, and left-sided weakness. On examination, she was drowsy with reactive pupils. The left upper and lower limbs exhibited flaccid paralysis with Medical Research Council (MRC) scale grade 0 strength. NCCT revealed an SAH, predominantly in the right Sylvian fissure. Conventional angiography identified an MCA aneurysm measuring 8 mm in length and 6.8 mm in transverse diameter. After adequate aneurysm coiling, occlusion of the distal ICA was noted. Full revascularization (TICI 3) was achieved using a Solitaire AB stent retriever (4 × 20 mm) (Fig. 5a-d). The occlusion time was 25 min until full recanalization was achieved. Upon discharge, she showed significant improvement in the motor strength of her lower limb (MRC scale grade 4), while the upper limb remained weak (MRC scale grade 1), resulting in an mRS score of 3. A small coil loop was observed protruding from the aneurysm sac (Fig. 5b); therefore, she was prescribed a single antiplatelet agent (aspirin 100 mg/day) for 1 month.
 Click for large image | Figure 5. Case 5. (a) Anteroposterior angiography showing middle cerebral artery aneurysm (red arrow). (b) Post coiling anteroposterior angiography with balloon remodeling (white arrow). (c) Anteroposterior angiography showing occluded distal internal carotid artery (green arrow). (d) Post mechanical thrombectomy anteroposterior angiography showing recanalized middle cerebral artery. |
Inclusion criteria
Case series describing thromboembolism causing flow arrest in major arteries during endovascular treatment of ruptured aneurysms were included.
Exclusion criteria
Cases of unruptured aneurysms or aneurysmal rupture occurring during thrombectomy for acute stroke management were excluded.
A literature review was conducted in the PubMed and Ovid Medline databases using the following keywords: “rescue”, “thrombectomy”, “ruptured aneurysms”, “subarachnoid hemorrhage”, and “acute”, in various combinations with AND/OR operators.
Ten studies (summarized in Table 2) were identified in the English literature [7-16]. A total of 34 cases of ruptured aneurysms complicated by major arterial occlusions, including five cases from our study, were analyzed, with a mean patient age of 52.7 years (18 males, 16 females).
 Click to view | Table 2. Patients Demographics and Clinical Outcome of the Reviewed Cases in the Literature |
Literature review
The aneurysms were located at the ACOM in 11 patients, PCOM in eight, MCA in five, basilar tip in three, ICA terminus in two, ICA in three, anterior choroidal (ANT CHOR) in one, and vertebral artery in one. Aneurysm sizes ranged from 1.9 to 13 mm. Thrombus developed distal to the aneurysm in 22 cases (64.7%), at the coil interface in four cases (11.7%), and proximal to the aneurysm in eight cases (23.5%). Simple coiling was the most frequently used technique, performed in 18 cases (61%), followed by balloon-assisted coiling in nine cases, stent-assisted coiling in four cases, and double microcatheter techniques in three cases.
The stent retriever technique was employed in 28 cases (82.3%), the aspiration technique in five cases, and the aspiration plus stent retriever (Solumbra) technique in one case. The time from thrombus development to recanalization ranged from 13 to 77 min, with one case of basilar occlusion accompanying a ruptured basilar tip aneurysm, which took 330 min for recanalization. Ten patients received intra-arterial fibrinolytic agents or glycoprotein (GP) IIb/IIIa inhibitors during the intervention. Angiographic recanalization was assessed using the TICI perfusion scale, achieving full recanalization (TICI 3) in 28 patients (82.3%), TICI 2B in four, and TICI 2A in two patients. Seven patients developed ischemic infarctions, as evidenced on follow-up CT scans. Hemorrhagic complications occurred in two patients who received intra-arterial tirofiban (5.8%), both of whom experienced neurological consequences and were discharged with an mRS of 2 and 3. Three patients died: two from ischemic complications and one from poor-grade SAH (grade V), unrelated to arterial occlusion. Twenty-two (64.7%) patients were discharged with mRS scores of 0 or 1, four with mRS 2, five with mRS 3, one with mRS 4, and three with mRS 6, while the status of one patient was not specified.
| Discussion | ▴Top |
Thromboembolism during endovascular treatment of cerebral aneurysms is the most common complication. In our database, 49 patients experienced thromboembolic complications between 2014 and 2023, accounting for 8.9% of cases. These complications can be categorized into three groups: 1) complete flow arrest in a major artery, 2) filling defect with maintained flow, and 3) distal small branch occlusion. This review specifically focuses on thromboembolic complications that result in complete flow arrest in a major artery. Previously, researchers have identified several risk factors for thromboembolism during endovascular treatment of cerebral aneurysms, including advanced age (over 65) [17], acutely ruptured aneurysms, aneurysm morphology, large size, neck width [18], and proximity to a large branch. Technical factors, such as the use of double microcatheters, balloon or stent-assisted techniques, procedure length, and operator experience, have also been discussed [19]. Lee et al highlighted that procedure time may be the most significant modifiable factor for reducing thromboembolic events, regardless of the technique or tools used during the coiling of cerebral aneurysms. However, we did not calculate the time from the start of the procedure until thrombus development in all cases, nor did we find relevant data in the reviewed studies [20]. One might expect that thrombus formation occurs more frequently with the use of adjuvant tools, such as balloons or double microcatheters. However, the data collected in this review show that 61% of cases involved the simple coiling technique. Another notable finding is that most thrombus-induced occlusions were not located at the coil-parent artery interface, with only 11% of the occlusion sites found in this location. In contrast, 64.7% of the occlusions were identified distal to the aneurysm. Thromboembolic complications are more prevalent during the treatment of ruptured cerebral aneurysms, as SAH induces a hypercoagulable state [21]. Additionally, antiplatelet agents are rarely used in the context of acute SAH. Distal arterial occlusion or thrombus formation resulting in a filling defect with maintained arterial flow is often treated with intra-arterial thrombolytic agents. However, in cases of complete arterial occlusion, the efficacy of intra-arterial thrombolytic or fibrinolytic agents may be limited. Mechanical thrombectomy has become an established standard treatment for acute ischemic stroke in adults with large vessel occlusion (LVO) [22]. However, the bridging technique, which involves the use of IV thrombolytic therapy in patients presenting within the first 4.5 h from symptom onset prior to thrombectomy, is still recommended by current guidelines for acute ischemic stroke treatment [22]. IV thrombolysis carries potential risks, including delays in thrombectomy, intracranial hemorrhage, and thrombus fragmentation. Moreover, Wong and colleagues identified IV thrombolysis as a predictor for emboli to distal or new territories [23]. A meta-analysis, conducted by Jang and colleagues, comparing the bridging technique to mechanical thrombectomy alone, demonstrated the non-inferiority of direct mechanical thrombectomy compared to the bridging technique in terms of functional independence, mortality, symptomatic intracranial hemorrhage (sICH), and successful recanalization [24]. The above recommendations apply to acute ischemic stroke with LVO. While it is challenging to directly apply these recommendations to our cases, the use of the bridging technique for acute thromboembolism causing major arterial occlusion during endovascular treatment of cerebral aneurysms should be reserved for cases in which the aneurysm is secured with coils.
Timely recanalization of the occluded artery in acute stroke is essential for determining functional outcomes, and this principle extends to interventions complicated by large arterial occlusions. Hence, mechanical thrombectomy appears to be an effective approach in cases of LVO caused by thromboembolism during endovascular treatment of cerebral aneurysms. Although it is ethically challenging to design a randomized trial comparing thrombectomy versus medical treatment in the pediatric age group, Findlay and colleagues conducted a meta-analysis and systematic review of studies involving 192 children treated with stent retrievers for large arterial occlusion. Even in the pediatric population, a high recanalization rate of 88.5% was observed, with a favorable clinical outcome achieved in 76.1% of cases [25].
The ACT should be maintained at twice the control level, targeting a range of 200 - 250 s during coiling. In our cohort, ACT was not measured in case 2, as thrombus formation occurred prematurely during the exchange for placing the guiding catheter, and it was unavailable in case 5. In the remaining three patients, the ACT did not reach the target value and was only measured after thrombus formation was detected. The recanalization rate was favorable in the reviewed cases, with 32 patients achieving TICI 3/2b recanalization, representing 94%. A favorable clinical outcome, regardless of SAH grading, was achieved in 61.7% of cases. There is a theoretical risk of destabilization and migration of the coil mass when using stent retrievers, especially if a coil loop protrudes into the arterial lumen. Neck injury and subsequent aneurysm bleeding are additional concerns associated with stent retriever use. However, no such complications were observed in any of the cases included in this study. Although aspiration techniques were used less frequently in the current study, they may theoretically provide a safer alternative in this context.
Our study has limitations typical of retrospective case series analysis, including missing data that may have provided additional insights, such as the influence of procedure duration and ACT levels at the time thrombus formation occurred. We also acknowledge the small sample size.
Conclusion
Mechanical thrombectomy for thromboembolic complications during endovascular treatment of acutely ruptured aneurysms appears to be an effective approach, facilitating rapid recanalization with a low incidence of hemorrhagic complications and obviating the need for intra-arterial lytic therapy. A randomized trial comparing direct mechanical thrombectomy to the bridging technique in the context of large arterial occlusion during endovascular treatment of cerebral aneurysms could provide valuable insights. In our perspective, this should be limited to cases where arterial occlusion occurs after the aneurysm has been successfully secured and sealed with coils. To further strengthen our understanding, randomized controlled trials (RCTs) using different mechanical thrombectomy techniques might be needed to establish an appropriate approach for managing such critical complications. In the meantime, creating a large, prospective, global multicenter registry to collect clinical data on strategies for addressing thromboembolic complications leading to large vessel occlusion during endovascular treatment of acutely ruptured aneurysms would be a valuable step forward.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no relevant conflict of interest to report.
Informed Consent
Informed consent was obtained from the patients or first-degree relatives.
Author Contributions
Mostafa Mahmoud: idea, literature review, manuscript writing, and overall responsibility. Ehab Mahmoud: editing, revision, and literature review. Osman Koc: editing, revision, and data collection. Ali Ayyad: manuscript editing, data collection, and revision. Suhail Hussain: revision and typographical editing. Ahmad Muhammad: revision, typographical and grammatical editing. Hassan Haroon: critical analysis and data collection. Yahia Imam: revision and manuscript editing. Ahmed Own: critical analysis and final approval.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ACOM: anterior communicating; ACT: activated clotting time; ANT CHOR: anterior choroidal; CT: computed tomography; ICA: internal carotid artery; MCA: middle cerebral artery; MRC: Medical Research Council; mRS: modified Rankin scale; NA: not available; NCCT: non-contrast CT; PCA: posterior cerebral artery; PCOM: posterior communicating; RCT: randomized controlled trial; rTPA: recombinant tissue plasminogen activator; SAH: subarachnoid hemorrhage; TICI: thrombolysis in cerebral infarction
| References | ▴Top |
- Soeda A, Sakai N, Sakai H, Iihara K, Yamada N, Imakita S, Nagata I. Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol. 2003;24(1):127-132.
pubmed - Brooks NP, Turk AS, Niemann DB, Aagaard-Kienitz B, Pulfer K, Cook T. Frequency of thromboembolic events associated with endovascular aneurysm treatment: retrospective case series. J Neurosurg. 2008;108(6):1095-1100.
doi pubmed - Ries T, Siemonsen S, Grzyska U, Zeumer H, Fiehler J. Abciximab is a safe rescue therapy in thromboembolic events complicating cerebral aneurysm coil embolization: single center experience in 42 cases and review of the literature. Stroke. 2009;40(5):1750-1757.
doi pubmed - Eskridge JM, Song JK. Endovascular embolization of 150 basilar tip aneurysms with Guglielmi detachable coils: results of the Food and Drug Administration multicenter clinical trial. J Neurosurg. 1998;89(1):81-86.
doi pubmed - Vinuela F, Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997;86(3):475-482.
doi pubmed - van Rooij WJ, Sluzewski M. Procedural morbidity and mortality of elective coil treatment of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2006;27(8):1678-1680.
pubmed - Hirata K, Yamazaki T, Kato N, Yasuda S, Matsumura A. Mechanical thrombectomy for occlusion near a ruptured intracranial aneurysm: A case report. Surg Neurol Int. 2020;11:120.
doi pubmed - Ahn JH, Jun HS, Song JH, Cho BM, Lee HK, Kim BC, Hyun DK, et al. Rescue mechanical thrombectomy using a retrievable stent for thromboembolic occlusion occurring during coil embolization of ruptured intracranial aneurysms. J Neurointerv Surg. 2017;9(3):244-249.
doi pubmed - Zhang X, Guo Z, Xu R, Sun X, Li Y. Mechanical thrombectomy in two patients using the Solitaire AB device in cerebral aneurysms during endovascular coil embolisation. J Clin Neurosci. 2012;19(12):1736-1738.
doi pubmed - Briganti F, Leone G, Marseglia M, Chiaramonte C, Solari D, Caranci F, Cappabianca P, et al. Mechanical thrombectomy in the treatment of distal occlusions during coil embolization of ruptured intracranial aneurysms. NMC Case Rep J. 2016;3(4):115-117.
doi pubmed - Drakopoulou M, Giannopoulou A, Zampakis P, Messinis L, Theofanopoulos A, Constantoyannis C, Panagiotopoulos VE. Suction thrombectomy using a microcatheter as a salvage method for acute distal occlusion during cerebral aneurysm embolization: A case report. Brain Circ. 2022;8(2):112-116.
doi pubmed - Kang DH, Kim YS, Park J, Hwang YH. Rescue forced-suction thrombectomy using the reperfusion catheter of the Penumbra System for thromboembolism during coil embolization of ruptured cerebral aneurysms. Neurosurgery. 2012;70(1 Suppl Operative):89-93; discussion 93-84.
doi pubmed - Domingo RA, Martinez Santos JL, Ravindran K, Tawk RG, We thank the ERG. Management of thromboembolic complications during aneurysm coiling: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2021;20(5):E348-E349.
doi pubmed - Aketa S, Wajima D, Kim T, Tei R, Yonezawa T. Coil embolization for ruptured basilar tip aneurysm after mechanical thrombectomy for acute basilar artery occlusion. World Neurosurg. 2016;93:488.e489-488.e412.
doi pubmed - Xu N, Meng H, Liu T, Feng Y, Qi Y, Wang H. Treatment of acute thromboembolic complication after stent-assisted coil embolization of ruptured intracranial aneurysm: a case report. Neuropsychiatr Dis Treat. 2019;15:69-74.
doi pubmed - Demartini Junior Z, Gatto LAM, Koppe GL, Oliveira T, Francisco AN. Rescue therapy with stent retrievers for thromboembolism during endovascular treatment of intracranial aneurysms. Arq Neuropsiquiatr. 2018;76(5):332-338.
doi pubmed - Cai Y, Spelle L, Wang H, Piotin M, Mounayer C, Vanzin JR, Moret J. Endovascular treatment of intracranial aneurysms in the elderly: single-center experience in 63 consecutive patients. Neurosurgery. 2005;57(6):1096-1102; discussion 1096-1102.
doi pubmed - Pierot L, Cognard C, Anxionnat R, Ricolfi F, Investigators C. Ruptured intracranial aneurysms: factors affecting the rate and outcome of endovascular treatment complications in a series of 782 patients (CLARITY study). Radiology. 2010;256(3):916-923.
doi pubmed - Kocur D, Pazdziora P, Przybylko N, Kukier W, Baron J, Rudnik A. Thromboembolism during coiling of intracranial aneurysms: predictors and clinical outcome. Wideochir Inne Tech Maloinwazyjne. 2020;15(2):319-328.
doi pubmed - Lee SH, Jang MU, Kang J, Kim YJ, Kim C, Sohn JH, Yang J, et al. Impact of reducing the procedure time on thromboembolism after coil embolization of cerebral aneurysms. Front Neurol. 2018;9:1125.
doi pubmed - van Rooij WJ, Sluzewski M, Beute GN, Nijssen PC. Procedural complications of coiling of ruptured intracranial aneurysms: incidence and risk factors in a consecutive series of 681 patients. AJNR Am J Neuroradiol. 2006;27(7):1498-1501.
pubmed - Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418.
doi pubmed - Wong GJ, Yoo B, Liebeskind D, Baharvahdat H, Gornbein J, Jahan R, Szeder V, et al. Frequency, determinants, and outcomes of emboli to distal and new territories related to mechanical thrombectomy for acute ischemic stroke. Stroke. 2021;52(7):2241-2249.
doi pubmed - Jang KM, Choi HH, Jang MJ, Cho YD. Direct Endovascular Thrombectomy Alone vs. Bridging Thrombolysis for Patients with Acute Ischemic Stroke : A Meta-analysis. Clin Neuroradiol. 2022;32(3):603-613.
doi pubmed - Findlay MC, Grandhi R, Nelson JR, Lucke-Wold B, Chowdhury MAB, Hoh BL, Steinberg J, et al. How do children fare compared with adults? Comparing relative outcomes after thrombectomy for acute ischemic stroke due to large-vessel occlusion. J Stroke Cerebrovasc Dis. 2023;32(11):107350.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.