| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://jnr.elmerpub.com |
Case Report
Volume 000, Number 000, October 2025, pages 000-000
Intimal Dissection Suspected to Be a Carotid Web That Resolved Spontaneously
Seigo Kimuraa, c, Daiji Ogawaa, Masahiro Hayashia, Norihito Fukawaa, Keiichi Yamadaa, Hirokatsu Taniguchia, Masahiko Wanibuchib
aKouzenkai Yagi Neurosurgical Hospital, Osaka, Osaka 537-0011, Japan
bOsaka Medical and Pharmaceutical University Hospital, Takatsuki City, Osaka 569-8686, Japan
cCorresponding Author: Seigo Kimura, Kouzenkai Yagi Neurosurgical Hospital, Osaka, Osaka 537-0011, Japan
Manuscript submitted June 11, 2025, accepted August 26, 2025, published online October 10, 2025
Short title: Intimal Dissection Suspected to Be a Carotid Web
doi: https://doi.org/10.14740/jnr1035
| Abstract | ▴Top |
The carotid web (CW) is a shelf-like structure in the posterior wall of the origin of the internal carotid artery (ICA). This report discusses a case wherein surgical treatment was planned for a lesion suspected to be a CW, but the lesion disappeared over time. A 32-year-old male was found collapsed and was admitted to our hospital. Diffusion-weighted magnetic resonance imaging revealed hyperintensity in the left middle cerebral artery. Three-dimensional computed tomography angiography (3D-CTA) and cerebral angiography revealed a shelf-like structure in the posterior wall of the origin of the left cervical ICA. This was diagnosed as left middle cerebral artery occlusion secondary to a CW, which was initially treated medically. Surgical treatment was planned after being transferred from a recovery hospital. However, approximately 3 months later, 3D-CTA and cerebral angiography revealed that the shelf-like structure on the posterior wall of the origin of the left cervical ICA had disappeared. This CW-like lesion may have been an intimal dissection which spontaneously resolved before complete formation of the CW.
Keywords: Carotid web; Intimal dissection; Hemodynamic change; Medical treatment
| Introduction | ▴Top |
The carotid web (CW) is a shelf-like structure located in the posterior wall of the origin of the internal carotid artery (ICA), and it is one of the causes of cerebral infarction in young patients [1, 2]. CWs can reportedly cause thrombus formation, leading to a high incidence of recurrent cerebral infarction [3]. Many cases have reported carotid endoarterectomy (CEA) for the management of CW [4, 5], although carotid artery stenting (CAS) is also becoming another popular option [6, 7]. However, cases wherein the CW disappears over time are extremely rare. This report describes a case wherein surgical treatment was planned for a lesion suspected to be a CW, but the lesion spontaneously disappeared over time.
| Case Report | ▴Top |
Investigations
A 32-year-old male was found collapsed in front of his home and brought to our hospital for emergency medical assistance. He had no remarkable past medical or family history. Upon arrival, the patient had a Glasgow Coma Scale (GCS) score of 10 (E3, V2, M5) with left conjugative deviation, total aphasia, and right hemiparesis. The National Institutes of Health Stroke Scale score was 20. The patient had an elevated blood pressure (151/95 mm Hg) and pulse rate (104/min).
Diagnosis
The electrocardiogram showed no evidence of atrial fibrillation. Diffusion-weighted image (DWI) of his head magnetic resonance imaging (MRI) revealed high intensity area of the left middle cerebral artery (MCA) area (Fig. 1a). T2* of his head MRI revealed a low intensity area in the left basal ganglia (Fig. 1b). Head magnetic resonance angiography (MRA) revealed loss of the left MCA (Fig. 1c). Cervical MRA showed no apparent stenosis (Fig. 1d). The patient was hospitalized and treated conservatively. Due to hemorrhage in the left basal ganglia, the patient was treated with edaravon (60 mg/day) without antithrombotic agents.
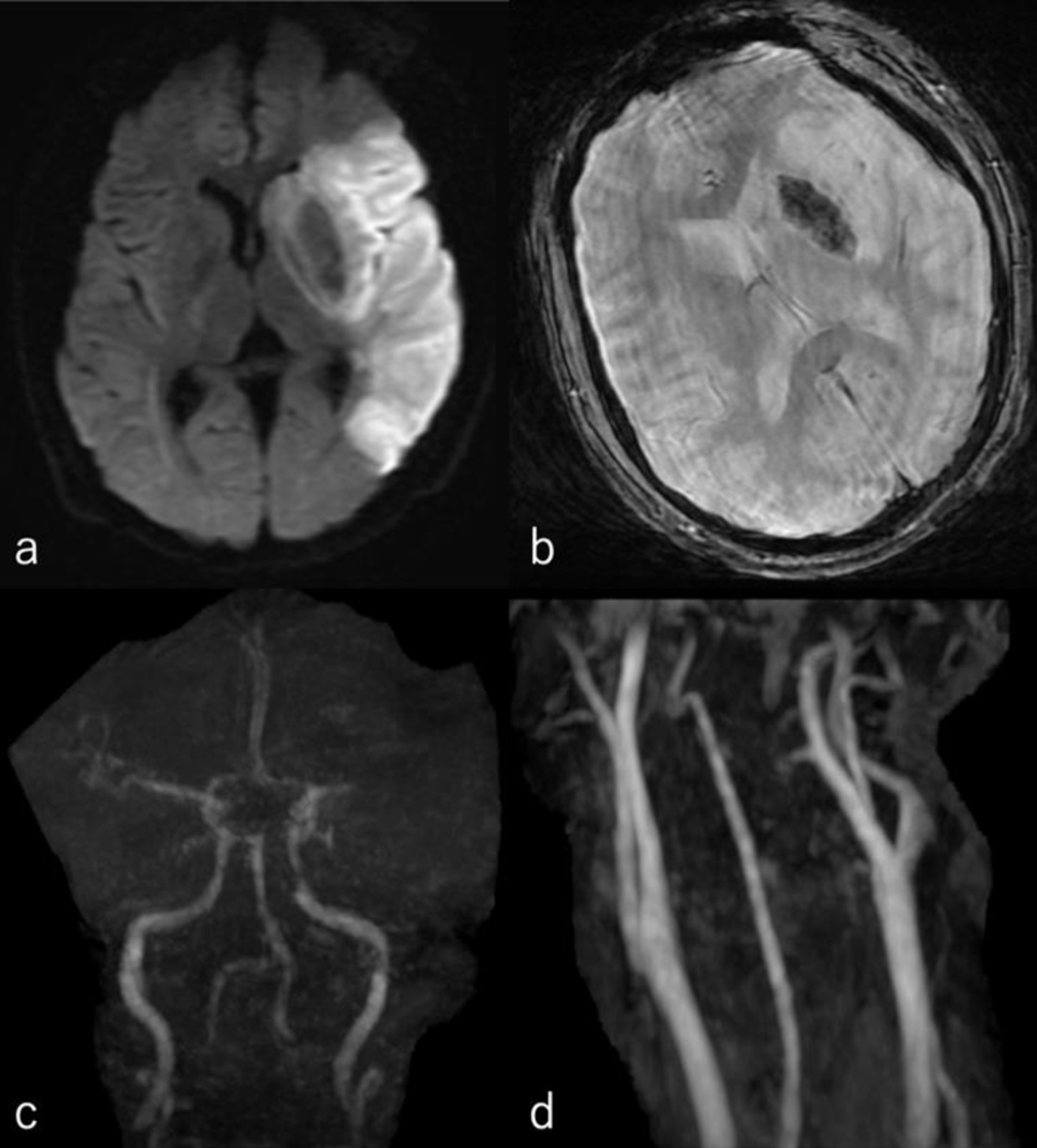 Click for large image | Figure 1. (a) Diffusion-weighted image of his head MRI revealed high intensity area of the left middle cerebral artery area. (b) T2* of his head MRI revealed a low intensity area in the left basal ganglia. (c) Head MRA revealed loss of the left middle cerebral artery. (d) Cervical MRA showed no apparent stenosis. MRA: magnetic resonance angiography; MRI: magnetic resonance imaging. |
The following day, no apparent hemorrhagic extension was observed. On carotid artery ultrasonography, there was a mobile lesion at the origin of the left ICA (Fig. 2). Further examination with three-dimensional computed tomography angiography (3D-CTA) revealed the presence of irregular contrast in the posterolateral wall of the left cervical ICA origin (Fig. 3a-d). MRI plaque image revealed a structure that was T1 isointense (Fig. 4a) and T2 high intense (Fig. 4b) with the vessel wall, protruding into the lumen (Fig. 4). On the second day, cerebral angiography revealed a shelf-like structure on the posterior wall of the left ICA origin (Fig. 5a), and the left MCA was recanalized. Cerebral angiography revealed pooling of blood flow on the rostral side of the lesion (Fig. 5b).
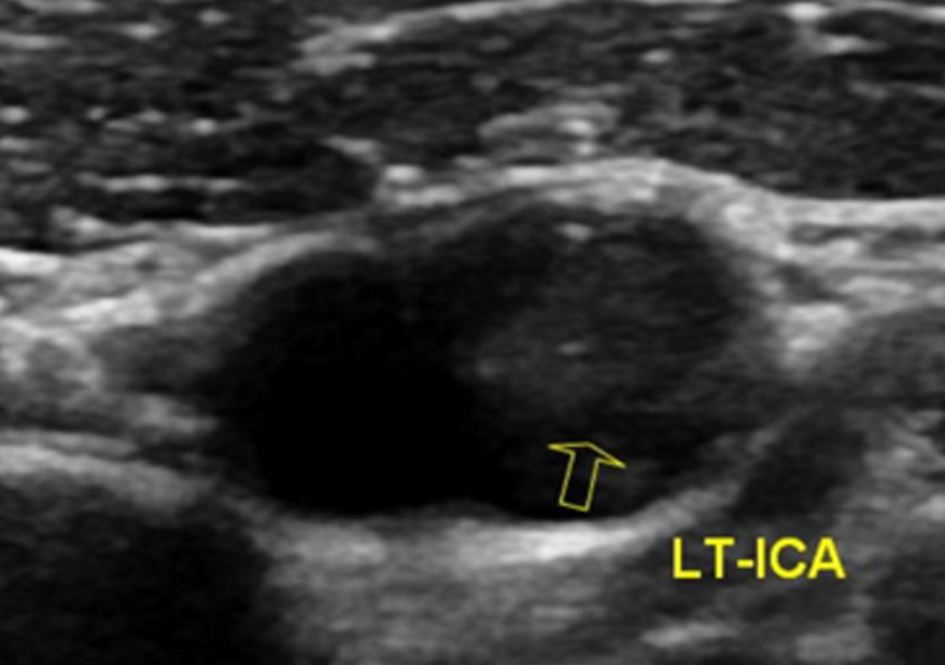 Click for large image | Figure 2. On carotid artery ultrasonography, there was a mobile lesion at the origin of the left internal carotid artery (yellow arrow). |
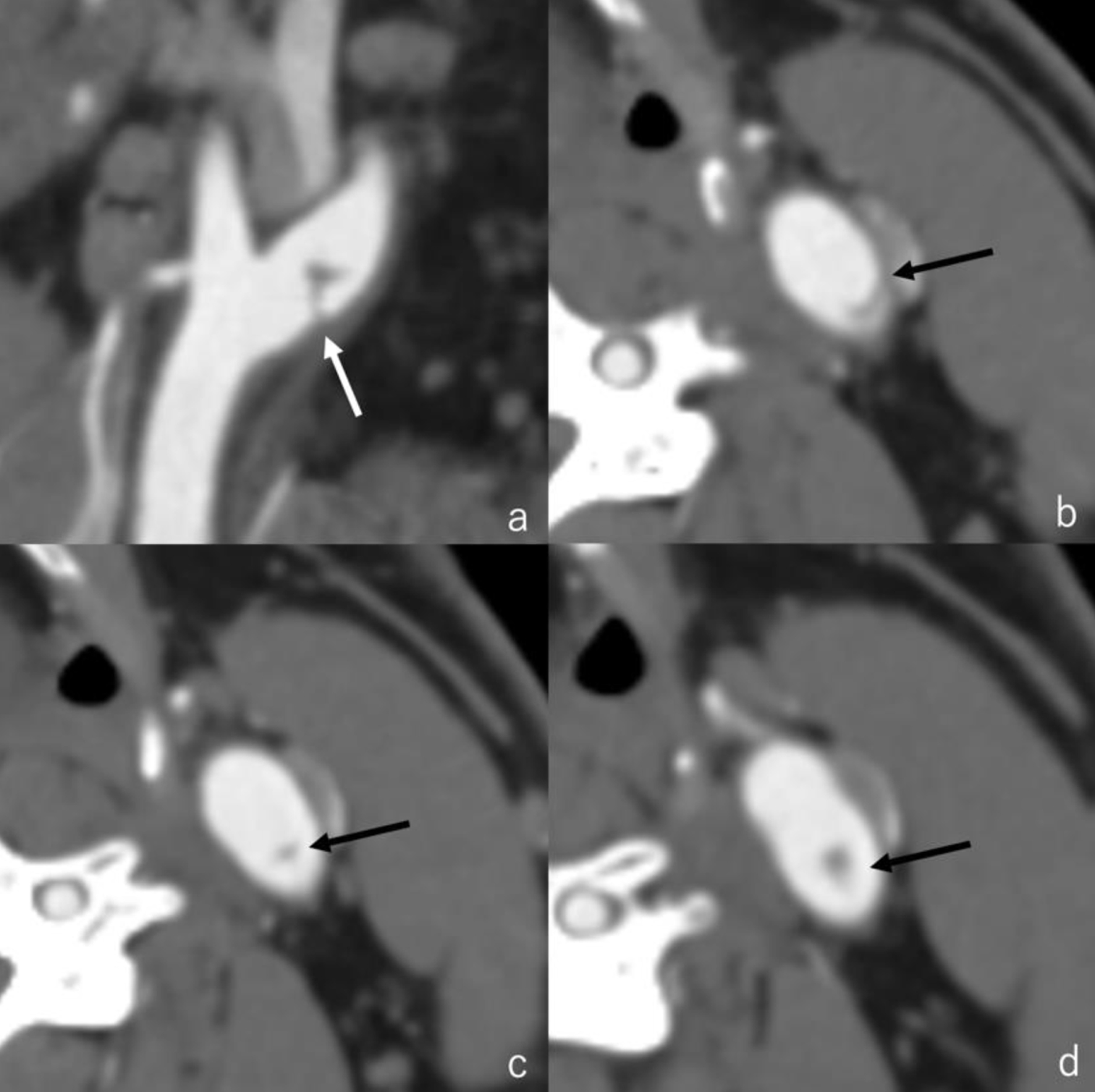 Click for large image | Figure 3. Three-dimensional computed tomography angiography revealed the presence of irregular contrast in the posterolateral wall of the left cervical internal carotid artery origin. (a) Sagittal image (white arrow); (b-d) axial images (black arrow). |
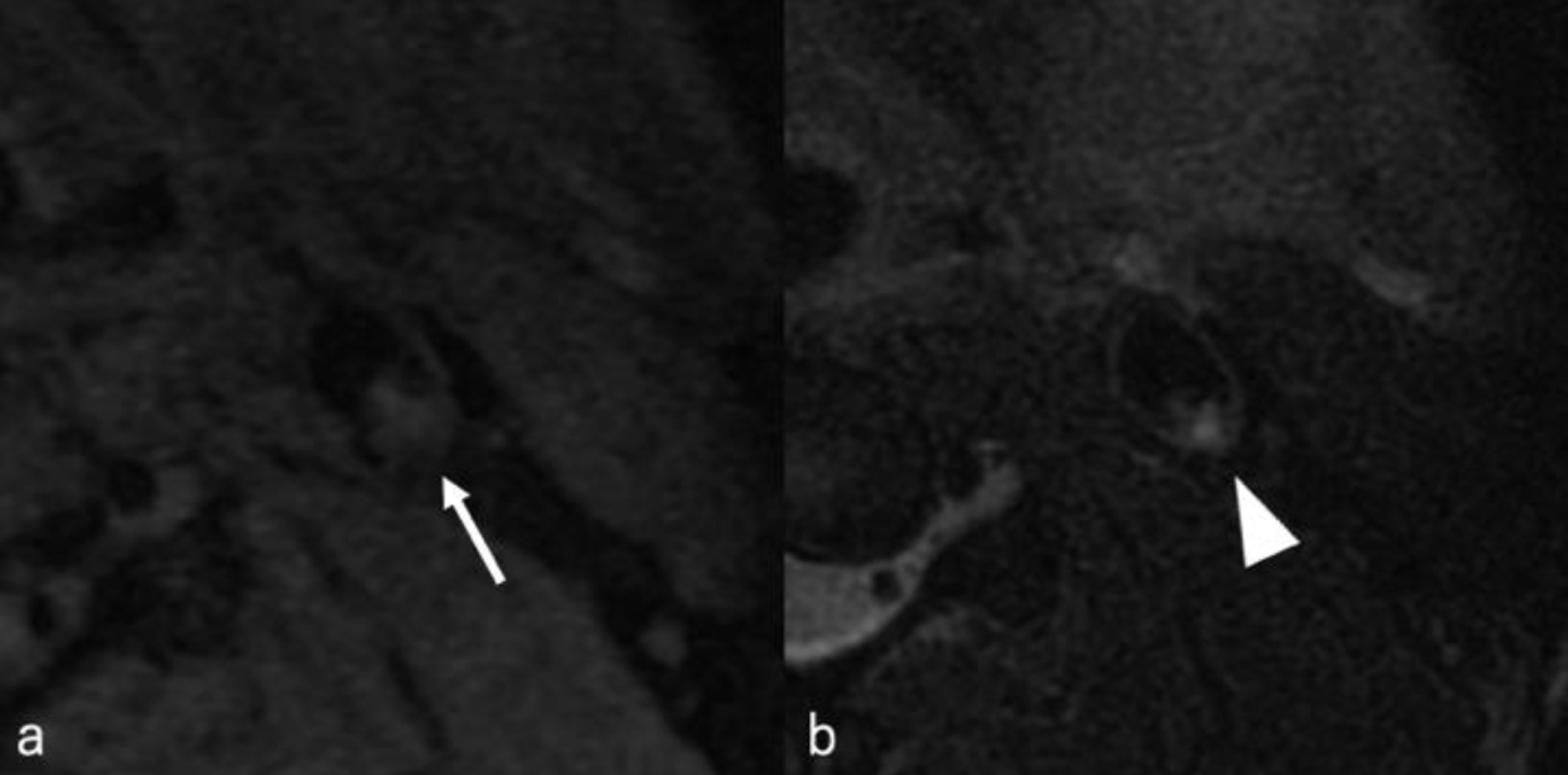 Click for large image | Figure 4. MRI plaque image revealed a structure that was T1 isointense (white arrow) (a) and T2 hyperintense (white arrowhead) (b) with the vessel wall, protruding into the lumen. MRI: magnetic resonance imaging. |
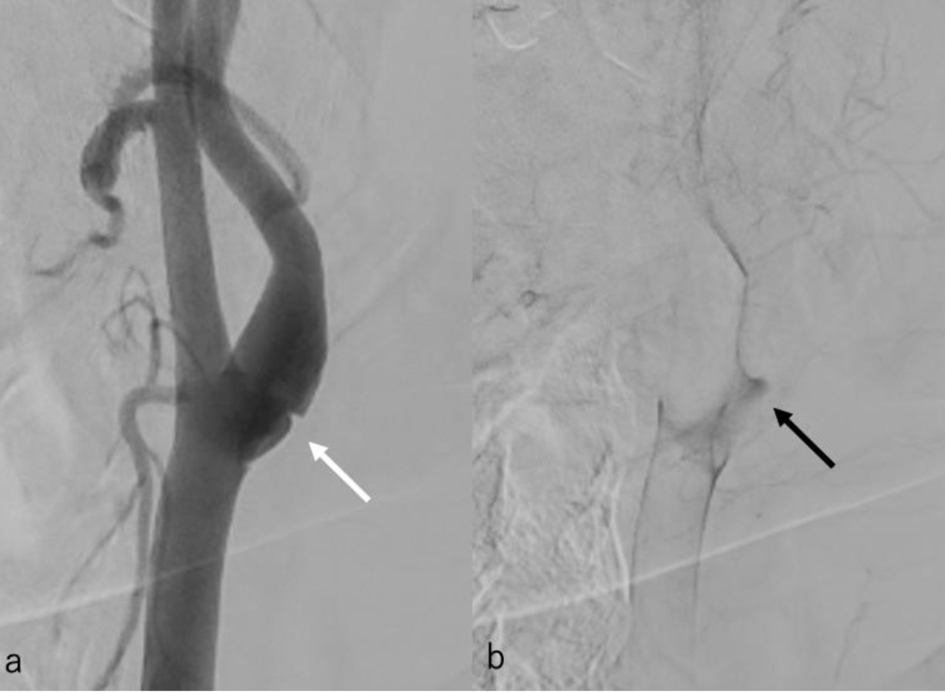 Click for large image | Figure 5. (a) Cerebral angiography revealed a shelf-like structure on the posterior wall of the left internal carotid artery origin on the second day. (b) Cerebral angiography revealed pooling of blood flow on the rostral side of the lesion. |
Based on the above imaging findings, the patient was diagnosed with cerebral infarction caused by CW.
Treatment
Two days after symptom onset, since there was no evidence of hemorrhagic expansion, the patient was given argatroban (60 mg/day for 2 days, followed by 20 mg/day for 5 days), clopidogrel (75 mg/day), and pitavastatin calcium (2 mg/day). Carotid artery ultrasonography performed 20 days after symptom onset showed that the mobile lesion attached to the CW had disappeared. There was no neurological aggravation, and the patient was transferred to a recovery hospital 41 days after symptom onset. At 85 days after symptom onset, the patient was transferred to our hospital for surgical treatment of the CW. A 3D-CTA performed 86 days after symptom onset showed that the shelf-like structure on the posterior wall of the origin of the left ICA had disappeared (Fig. 6), which was further confirmed on cerebral angiography performed the following day (Fig. 7). We considered that either the CW had disappeared or the intimal dissection had repaired spontaneously, and thus, surgical treatment was not performed.
 Click for large image | Figure 6. Three-dimensional computed tomography angiography performed 86 days after symptom onset showed that the shelf-like structure on the posterior wall of the origin of the left internal carotid artery had disappeared. |
 Click for large image | Figure 7. Cerebral angiography performed 87 days after symptom onset showed that the shelf-like structure on the posterior wall of the origin of the left internal carotid artery had disappeared. |
Follow-up and outcomes
The patient was discharged from our hospital 100 days after symptom onset, with a GCS of 13 (E4, V3, M6) and a modified Rankin Scale score of 3.
| Discussion | ▴Top |
CW is a subtype of fibromuscular dysplasia wherein the pathological tissue shows few changes in the media and is mainly characterized by fibrous hyperplasia of the intima [4, 8]. The diagnosis of CW is often based on morphology as seen on radiographic imaging. Cerebral angiography and CTA are useful diagnostic tools [9], typically revealing a contrast defect caused by a shelf-like structure on the posterior wall of the origin of the ICA, with blood flow pooling on the rostral side of the structure [7, 10]. This pooling of the blood promotes thrombus formation, which can result in cerebral infarction [1]. In the present case, CTA revealed a shelf-like structure on the posterolateral wall of the origin of the ICA, and this was also seen on cerebral angiography, alongside blood flow pooling on the rostral side of the structure. These imaging findings are strongly suggestive of CW.
CW has a relatively low detection rate on carotid artery echocardiography. Joux et al [8] noted that in 18 of 21 cases, CW was not obvious and could be misdiagnosed as fibrous plaques since the findings were nonspecific. Thomas et al [9] demonstrated the superiority of cerebral angiography and CTA compared with carotid artery echocardiography in the diagnosis of CW. In the present case, we were able to identify a thrombus that seems to be attached to the lesion, but the lesion itself could not be observed. On MRI plaque image, the structure of CW typically has a continuous signal with the vessel wall that protrudes into the lumen from the posterior wall of the origin of the ICA [6, 11]. The same MRI findings were observed for this patient. Reportedly, the CW intensity on MRI plaque imaging typically appears as T1 isointense and T2 hyperintense signals [12, 13]. Herein, the areas identified as CW showed T1 isointensity and T2 hyperintensity, consistent with previous findings. In contrast, the areas identified as attached thrombus demonstrated T1 isointensity and T2 hypointensity. Kimura et al [12] presented a case wherein an attached thrombus disappeared over time; the thrombus showed T1 and T2 isointensity, whereas the CW region revealed T1 isointensity and T2 hyperintensity. Although the signal intensity of the thrombus in our case slightly differs from that report, the CW intensity pattern remains consistent. Furthermore, MRI in our case revealed a hemorrhagic infarction in the left MCA region. The mechanism underlying the hemorrhagic infarction may include the presence of a thrombus in the proximal M1 segment, potentially including the perforating arteries. As the thrombus migrated distally along the M1, transient reperfusion of the perforators may have led to hemorrhagic changes.
Other than CW, the differential diagnoses for shelf-like structures in the posterior wall of the origin of the ICA may include arterial dissection and vasculitis. Cerebral artery dissection can result in stroke due to luminal narrowing or aneurysmal dilation, and patients clinically manifest with headache, neck pain, and facial pain. The typical imaging findings include the pearl and string sign, intimal flap sign, and double lumen sign on cerebral angiography. These clinical and radiographic findings are relatively specific for arterial dissection, which is confirmed by MRI and MRA. Notably, the imaging findings of the dissection often change within a short period of time during the acute phase, and remodeling also occurs over time [14]. Moreover, cerebral artery dissection shows high intensity on T1 plaque images while accompanied by an intramural thrombus in the dissection cavity [15].
Vasculitis is a general term for conditions that involve inflammation of the blood vessel walls, including independent diseases wherein vasculitis itself is the primary lesion (i.e., primary vasculitis) and cases wherein vasculitis accompanies other diseases (i.e., secondary vasculitis). Additionally, this may be accompanied by an unknown fever and a high inflammatory response [16]. Secondary vasculitis can be associated with other collagen diseases, inflammatory bowel disease, infections, drugs (e.g., antibiotics, allopurinol, thiazides, propiothiouracil, biologics, etc.), tumors, or transplants [17]. In the present case, there were no obvious imaging findings (i.e., pearl and string sign, double lumen sign). Moreover, the dissection cavity did not exhibit high intensity on T1-weighted MRI plaque images, potentially because of the small sample size of the lesion, which could have prevented the formation of an intramural thrombus, thereby resulting in the absence of T1 hyperintensity. Thus, it was not considered to be a typical arterial dissection. However, since the patient had aphasia, subjective complaints such as headache or neck pain could not be elicited, making it difficult to completely rule out a typical arterial dissection. The patient had no apparent collagen disease and no other significant medical history. There were no obvious medications that could have caused infection or vasculitis, nor was there unknown fever or markedly elevated C-reactive protein levels, making vasculitis unlikely. Based on the above, CW was strongly suspected in this case.
CW is generally believed to be a congenital/developmental lesion rather than an acquired lesion, although this has been controversial [18, 19]. In contrast, a few reports have indicated that CWs were not present at the time of initial diagnosis but were formed later on. Singh et al [20] reported a 43-year-old woman who had no CW seen on CTA, but at age 50, the presence of a CW was confirmed, which persisted until age 53. In that case, CW was considered to be an acquired lesion. Similarly, Vercelli et al [21] found no obvious abnormalities of the head and neck vessels on CTA in a 47-year-old man, but at age 49, workup for left hemiparesis revealed a CW in the posterolateral wall of the right ICA, which persisted until age 50. In that case, wall shear stress caused weakness of the posterolateral wall at the ICA bifurcation, resulting in endothelial vulnerability, and the endothelial reaction to these hemodynamic changes in the carotid bulb likely caused local intimal dissection. Thus, they considered that an intimal dissection can morphologically evolve into a CW and undergo reactive phenomena, creating a trapped area of fibrous tissue within the media. In contrast, the present case followed the opposite course, wherein an initial lesion that was suspected to be a CW eventually disappeared over time. We suspect that an initial intimal dissection resulted in the formation of this CW-like lesion, but the CW may not have formed completely. The intimal dissection may have been in the process of remodeling. Follow-up digital subtraction angiography (DSA) showed resolution of the CW-like lesions; however, wall irregularities were observed in the posterior wall of the ICA, potentially indicating a remodeling process after arterial dissection. Given that wall shear stress can weaken the posterolateral wall at the ICA bifurcation, potentially leading to local intimal dissection, anatomical features, such as the bifurcation angle of the ICA and the presence or absence of bulb dilatation, may serve as useful screening criteria for CW-like lesions. Moreover, CW is generally considered a potential cause of unexplained cerebral infarction in young individuals. Even without chronic hypertension, transient blood pressure elevation caused by exercise or straining can damage vascular endothelium. External mechanical forces to the neck may also be a risk factor for CW formation. However, this hypothesis remains purely theoretical because no specimen was collected for further pathological examination.
Medical treatment for CW typically has a high recurrence rate, whereas treatment with either CEA or CAS is highly effective [5], with CAS increasingly being chosen in the West due to its less invasive nature [22]. However, the pathologic diagnosis of CW can only be confirmed in CEA, because CAS does not involve collecting specimen for histological examination. Therefore, previous reports of CAS for CW exclusively rely on a radiographic diagnosis [10, 11]. Similarly, in the present case, CW was diagnosed based on radiological imaging only. CAS or CEA was planned for this patient, but surgical treatment was deferred since the lesion spontaneously disappeared. Although CEA could have enabled a pathological diagnosis, there were ethical concerns regarding the surgical removal of a lesion that had already disappeared. To the best of our knowledge, no previous reports have described shelf-like structures on the posterior wall of the origin of ICA that disappeared over time. Although the detailed pathological background of this lesion is unknown, the changes in radiographic findings over time in this case remain significant.
Learning points
A shelf-like structure in the posterior wall of ICA may be diagnosed as CW by 3D-CTA or cerebral angiography, but this can disappear over time. Such CW-like lesions could be the result of an intimal dissection wherein a CW was not completely formed and may have been in the process of remodeling.
Conclusion
This case report describes a lesion suspected to be a CW that spontaneously disappeared over time. The formation of this CW-like lesion was suspected to be due to an intimal dissection in the posterior wall of the origin of the ICA, which likely repaired without complete formation of the CW.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consent has been obtained from the patient for publication.
Author Contributions
Conceptualization, design, definition of intellectual content, literature search, clinical studies, data acquisition, data analysis, manuscript preparation, manuscript editing, and manuscript review: SK, DO, MH, NF, KY, HT, and MW. Guarantor: SK.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CAS: carotid artery stenting; CEA: carotid endoarterectomy; CW: carotid web; DWI: diffusion-weighted image; GCS: Glasgow Coma Scale; ICA: internal carotid artery; MCA: middle cerebral artery; MRA: magnetic resonance angiography; MRI: magnetic resonance imaging; 3D-CTA: three-dimensional computed tomography angiography
| References | ▴Top |
- Haussen DC, Grossberg JA, Bouslama M, Pradilla G, Belagaje S, Bianchi N, Allen JW, et al. Carotid web (Intimal Fibromuscular Dysplasia) has high stroke recurrence risk and is amenable to stenting. Stroke. 2017;48(11):3134-3137.
doi pubmed - Patel SD, Otite FO, Topiwala K, Saber H, Kaneko N, Sussman E, Mehta TV, et al. Interventional compared with medical management of symptomatic carotid web: A systematic review. J Stroke Cerebrovasc Dis. 2022;31(10):106682.
doi pubmed - Brinjikji W, Agid R, Pereira VM. Carotid stenting for treatment of symptomatic carotid webs: a single-center case series. Interv Neurol. 2018;7(5):233-240.
doi pubmed - Choi PM, Singh D, Trivedi A, Qazi E, George D, Wong J, Demchuk AM, et al. Carotid Webs and Recurrent Ischemic Strokes in the Era of CT Angiography. AJNR Am J Neuroradiol. 2015;36(11):2134-2139.
doi pubmed - Zhang AJ, Dhruv P, Choi P, Bakker C, Koffel J, Anderson D, Kim J, et al. A systemic literature review of patients with carotid web and acute ischemic stroke. Stroke. 2018;49:2872-2876.
- Tanaka Y, Takano H, Namekawa M, Suzuki T, Genkai N, Abe H. Carotid web stenting: a case report. Jpn J Stroke. 2021;43:256-261.
- Haussen DC, Grossberg JA, Koch S, Malik A, Yavagal D, Gory B, Leesch W, et al. Multicenter experience with stenting for symptomatic carotid web. Interv Neurol. 2018;7(6):413-418.
doi pubmed - Joux J, Chausson N, Jeannin S, Saint-Vil M, Mejdoubi M, Hennequin JL, Deschamps L, et al. Carotid-bulb atypical fibromuscular dysplasia in young Afro-Caribbean patients with stroke. Stroke. 2014;45(12):3711-3713.
doi pubmed - Madaelil TP, Grossberg JA, Nogueira RG, Anderson A, Barreira C, Frankel M, Haussen DC. Multimodality Imaging in Carotid Web. Front Neurol. 2019;10:220.
doi pubmed - Fukumoto H, Yoshinaga T, Morishita T, Fukuda K, Abe H, Sato K, Higashi T, et al. Diagnosis and treatment of carotid web: case report. Jpn J Stroke. 2021;43:360-364.
- Otsuka T, Kumai J, Ono Shingo, Takeda T. Two cases of carotid artery stenting in patients with recurrent cerebral embolism caused by a carotid web. Jpn J Stroke. 2023;45:348-354.
- Kimura S, Fukawa N, Hayashi M, Ogawa D, Yamada K, Taniguchi H, Wanibuchi M. Carotid artery stenting for a carotid web revealed by shape change after adherent thrombus resolution following conservative treatment. Surg Neurol Int. 2025;16:264.
doi pubmed - Onuki A, Kobayashi Y, Kameno R, Fujimori D, Munakata R, Horiuchi K, Oinuma M, et al. A case of artery stenting for carotid web diagnosed at the time of recurrence of embolic ischemic stroke. Jpn J Stroke. 2024;46:316-320.
- Goto A. Cerebral artery dissection (in Japanese). Nihon Naika Gakkai Zasshi (Journal of the Japanese Society of Internal Medicine). 2009;98(6):1311-1318.
- Edjlali M, Roca P, Rabrait C, Naggara O, Oppenheim C. 3D fast spin-echo T1 black-blood imaging for the diagnosis of cervical artery dissection. AJNR Am J Neuroradiol. 2013;34(9):E103-106.
doi pubmed - Wakisaka K, Hagiwara N, Kanazawa Y, Arakawa S, Ago T, Kitazono T. [Case of CNS-limited ANCA-associated vasculitis presenting as recurrent ischemic stroke]. Rinsho Shinkeigaku. 2014;54(5):429-433.
doi pubmed - Ozaki S. Diagnosis and treatment in clinical practice (in Japanese). Nihon Naika Gakkai Zasshi (Journal of the Japanese Society of Internal Medicine). 2007;96(12):2177-2188.
- Momose KJ, New PF. Non-atheromatous stenosis and occlusion of the internal carotid artery and its main branches. Am J Roentgenol Radium Ther Nucl Med. 1973;118(3):550-566.
doi pubmed - McNamara MF. The carotid web: a developmental anomaly of the brachiocephalic system. Ann Vasc Surg. 1987;1(5):595-597.
doi pubmed - Singh RJ, Mandell DM, Menon BK, Appireddy R. De novo formation of a carotid web in an adult: A longitudinal observation. J Stroke Cerebrovasc Dis. 2024;33(11):108010.
doi pubmed - Vercelli GG, Campeau NG, Macedo TA, Dawson ET, Lanzino G. De novo formation of a carotid web: case report. J Neurosurg. 2019;131(5):1481-1484.
doi pubmed - Guglielmi V, Compagne KCJ, Sarrami AH, Sluis WM, van den Berg LA, van der Sluijs PM, Mandell DM, et al. Assessment of recurrent stroke risk in patients with a carotid web. JAMA Neurol. 2021;78(7):826-833.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.