| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://jnr.elmerpub.com |
Original Article
Volume 15, Number 4, December 2025, pages 165-171
Blood Pressure Variability in Thrombectomy for Acute Ischemic Stroke: Post-Hoc Analysis of the BP-TARGET trial
Walter W. Merrimana, d , Mikael Mazhigib, David Z. Rosec, Adnan I. Qureshia
aZeenat Qureshi Stroke Institutes and Department of Neurology, University of Missouri, Columbia, MO, USA
bNeurology Department, Hopital Lariboisiere, Paris, France
cDepartment of Neurology, University of South Florida Morsani College of Medicine, Tampa, FL, USA
dCorresponding Author: Walter Merriman, Zeenat Qureshi Stroke Institutes and Department of Neurology, University of Missouri, Columbia, MO 65201, USA
Manuscript submitted September 18, 2025, accepted December 12, 2025, published online December 24, 2025
Short title: Blood Pressure Variability in BP-TARGET
doi: https://doi.org/10.14740/jnr1045
| Abstract | ▴Top |
Background: Factors associated with blood pressure variability (BPV) in acute ischemic stroke (AIS) patients undergoing thrombectomy have not been well established. Therefore, we performed a post-hoc analysis of the BP-TARGET trial, evaluating the relationship between BPV, post-procedural intraparenchymal hemorrhage (IPH), and functional independence at 90 days.
Methods: For 24 h after thrombectomy, blood pressure values were recorded and BPV was quantified by calculating the following indices: 24-h average real variability (AVR24), time rate index (TRI), successive variability (SV), standard deviation (SD), and range for systolic, diastolic, and mean arterial blood pressures. We assessed the effect of initial National Institutes of Health Stroke Scale (NIHSS) score, age, modified Thrombolysis in Cerebral Infarction (mTICI) score, and initial systolic blood pressure post-procedure on BPV, as well as the effect of BPV on IPH at 24 h and functional independence defined as modified Rankin Scale (mRS) of 0-2 at 90 days.
Results: A total of 193 AIS patients (mean age 72.7 ± 13.6 years), with an average post-procedure systolic blood pressure of 152.8 ± 25.6 mm Hg, were analyzed. An mTICI score of 2b (incomplete/subtotal recanalization), compared with mTICI score of 3 (full recanalization), predicted increased BPV (ARV: P = 0.014, TRI: P = 0.028, and SV: P = 0.030). There was no association between BPV and functional independence at 90 days (ARV: P = 0.185, TRI: P = 0.657, and SV: P = 0.550), or BPV and post-procedural IPH.
Conclusion: In this post-hoc analysis of the BP-TARGET trial, better recanalization was associated with decreased BPV in AIS patients post-thrombectomy. Nevertheless, we found no association between BPV indices and functional independence at 90 days or post-procedural IPH.
Keywords: Ischemic stroke; Blood pressure; Thrombectomy; Cerebral hemorrhage; Recanalization
| Introduction | ▴Top |
Intraparenchymal hemorrhage (IPH) after thrombectomy in patients with acute ischemic stroke (AIS) remains a major cause of death or disability [1]. Elevated systolic blood pressure (SBP) has been implicated in IPH pathophysiology after intravenous thrombolysis in AIS [2-6]. Subsequently, several clinical trials [7-10] have evaluated the role of SBP reduction in AIS patients undergoing thrombectomy. A meta-analysis of eight studies with 2,922 patients did not identify a difference in functional independence (defined as modified Rankin Scale (mRS) 0-2) at 90 days or IPH within 24 h in AIS patients with either intensive SBP reduction or moderate SBP reduction compared with standard SBP reduction post-thrombectomy [11]. Now, therefore, the focus may be shifting from absolute SBP values to blood pressure variability (BPV) as the most relevant biomarker associated with IPH and functional outcomes in AIS patients undergoing thrombectomy. Another meta-analysis demonstrated that increased variability of SBP in the acute phase, post-thrombectomy is associated with worse functional outcomes [12]. However, no consensus exists on which indices of BPV can or should be used for the purpose of quantifying increased BPV, or what magnitude of BPV is clinically relevant. The present study investigates the relationship between several indices of BPV and IPH and functional outcomes in AIS patients undergoing thrombectomy, and seeks to identify predictors of BPV, in a post-hoc analysis of a major multicenter randomized clinical trial [7].
| Materials and Methods | ▴Top |
Study population
We performed a post-hoc analysis of the BP-TARGET study, which was a multi-center trial that randomized AIS patients post-thrombectomy to either intensive SBP control (goal 100 - 129 mm Hg) or standard control (goal 130 - 185 mm Hg) [7]. Briefly, all patients within the BP-TARGET trial underwent thrombectomy for large vessel occlusion (LVO) in either the internal carotid artery or proximal middle cerebral artery (M1) within 6 h of symptom onset and achieved a modified Thrombolysis in Cerebral Ischemia (mTICI) score of 2b or 3 [13]. Investigators were permitted to use any antihypertensive agent, with calcium channel blockers being the most frequent choice. SBP and diastolic blood pressure (DBP) were recorded at the completion of thrombectomy, then every 15 min for 2 h, then every 30 min for 6 h, and then every hour until the 24 h mark. We only excluded patients who were missing: 1) > 20% of blood pressure (BP) recordings; 2) an initial SBP measurement; or 3) IPH data.
BP variables
Mean arterial pressure (MAP) was calculated using Gauer’s method [14]. BPV was assessed for each patient by calculating the following indices: 24-h apparent real variability (AVR24), time rate index (TRI), successive variability (SV), standard deviation (SD), ranges for SBP and DBP, and MAPs over the first 24 h post-thrombectomy. In all cases of missing BP data, the time index of the missing data was removed and the next index with available BP data was used.
The AVR24 is a time-weighted average of changes in BP, as previously described in the literature [15]. It is calculated by first multiplying the difference between two BP measurements (P) by the interval of time between them (wk), these values are then summated, and finally divided by the sum of the time intervals. The AVR24 equation is:
The TRI is an average rate of change between individual BP measurements [16]. It is calculated by finding the difference between measurements, then dividing that difference by the time (t) interval between them, then taking the average of that quotient. The TRI equation is:
SV is an averaged squared difference between adjacent BP measurements [17]. It is calculated by finding the squared difference between sequential BP measurements, then taking the average of those differences, and finally the square root of the average. The difference between SV and SD is that the former compares adjacent values, and the latter compares values to the mean. The SV equation is:
Outcomes
We analyzed the relationship of BPV variables with two outcomes: 1) post-thrombectomy IPH, defined as any new intraparenchymal hyperdensity consistent with hemorrhage on computed tomography (CT) obtained between 24 and 36 h post-procedure and verified on CT at 72 h post-procedure (regardless of symptoms); and 2) functional independence at 90 days, defined by a mRS score of 0-2. The mRS scoring at 90 days post-thrombectomy was ascertained by independent qualified personnel who did not participate in the randomization or in-hospital treatment of the patients.
Statistical analysis
The baseline characteristics of the sample population were expressed as a number for categorical variables and as a mean ± SD for continuous variables. We used a Welch t-test of independent means to compare the means of ARV24, TRI, SV, range, and SD between those patients with and without post-thrombectomy IPH. We utilized a multiple linear regression to determine which factors predicted the systolic ARV, TRI, and SV among independent variables of initial National Institutes of Health Stroke Scale (NIHSS), age, initial SBP, and mTICI score. The initial NIHSS scores were first converted from a raw score into levels of scores 0 to 9, 10 to 19, and 20 or more and included as an ordinal variable. The TICI scores of 2b and 3 were included as an ordinal variable. The initial SBP and age were included as continuous variables. A P-value of < 0.05 was considered significant. All data reduction and calculations were performed using the statistical programming language R (R Core Team (2024). _R: A Language and Environment for Statistical Computing_. R Foundation for Statistical Computing, Vienna, Austria [18]).
The research and preparation of this manuscript was determined to not be human subject research by University of Missouri Internal Review Board, and therefore not subject to approval by the same. The research and preparation of this manuscript adhered to ethical guidelines of the institution at which it was performed.
| Results | ▴Top |
The BP-TARGET study recruited 318 patients. After applying our exclusion criteria, 193 patients were identified for this post-hoc analysis. The most common reason for exclusion was BP data missing values exceeding 20% (n = 77), followed by mRS data missing at 90 days (n = 24), initial BP value missing (n = 19), and/or missing IPH data (n = 5). The mean patient age was 73 ± 14 years and 91 patients were men and 102 were women. Clinical characteristics are listed in Table 1. The mean initial NIHSS score (± SD) was 16 ± 6. Post-procedure, 83 patients had a TICI score of 2b (incomplete/subtotal recanalization) and 110 had a score of 3 (complete recanalization). The mean initial SBP was 153 ± 26 mm Hg. Post-thrombectomy IPH was seen in 77 (39.9%) of 193 patients (42.2% with mTICI 2b and 38.1% with mTICI 3) and functional independence at 90 days was seen in 98 of 193 patients (38.8% with mTICI 2b and 50.8% with mTICI 3).
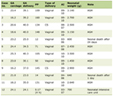 Click to view | Table 1. Baseline Characteristics for 193 Patients With Successful Thrombectomy of a Large Arterial Occlusion According to the Presence or Absence of Intraparenchymal Hemorrhage in the First 24 h Post-Procedure in a Post-Hoc Analysis of BP-TARGET Trial Data |
Predictors of BPV
A multiple linear regression was performed to identify factors that predicted systolic BPV. Among ARV24, TRI, and SV, a mTICI score of 3 (P = 0.014, P = 0.028, and P = 0.030, respectively) predicted a lower systolic BPV (Table 2). Pre-procedural NIHSS was also found to predict lower systolic BPV in TRI only (P = 0.028). Post-procedural initial SBP and age were not found to be significant predictors of BPV.
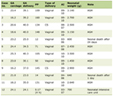 Click to view | Table 2. Multiple Linear Regression Model Results for 193 Patients With Successful Thrombectomy of a Large Arterial Occlusion for Prediction of Apparent Real Variability, Time Rate Index, and Successive Variability of Systolic Blood Pressure in the First 24 h Post-Procedure in a Post-Hoc Analysis of BP-TARGET Trial Data |
BP variables and post-thrombectomy IPH
Both a higher initial NIHSS (16.8 vs. 15.0, P = 0.044) and a lower rate of functional independence at 90 days (39.0% vs. 58.6%, P < 0.001) were found in patients with post-thrombectomy IPH compared to those without IPH (Table 1).
Calculations of ARV24, TRI, SV, range, and SD were performed for SBP, DBP, and MAPs for all patients. No significant deviations from the planned analysis were required. No significant relationship between indices of BPV and IPH was found in this analysis (Table 3).
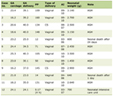 Click to view | Table 3. Measures and Significance of Indices of Blood Pressure Variability for 193 Patients With Successful Thrombectomy of a Large Arterial Occlusion According to the Presence or Absence of Intraparenchymal Hemorrhage in the First 24 h Post-Procedure in a Post-Hoc Analysis of BP-TARGET Trial Data |
BP variables and functional independence at 90 days
None of the indices of BPV tested were found to predict functional independence at 90 days (Table 4).
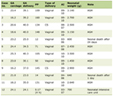 Click to view | Table 4. Multiple Linear Regression Model Results for 193 Patients With Successful Thrombectomy of a Large Arterial Occlusion for Prediction of Functional Independence at 90 days Based on Blood Pressure Variability Indices in the 24 h Post-Procedure, in a Post-Hoc Analysis of BP-TARGET Trial Data |
| Discussion | ▴Top |
The relationship between mTICI grades and three separate indices of BPV was evaluated in our post-hoc analysis of the BP-TARGET study, which was a multi-center trial that randomized AIS patients post-thrombectomy to either intensive SBP control (goal 100 - 129 mm Hg) or standard control (goal 130 - 185 mm Hg). A previous study showed that an incomplete revascularization (mTICI score < 3) is associated with greater BPV [19]. This is in keeping with the idea that to support retrograde flow through collateral blood vessels, and augment cerebral perfusion pressure (CPP), such incomplete reperfusion drives higher systemic pressure values and by extension increases BPV [11].
In a recent meta-analysis of 11 studies comprising 3,520 patients, BPV was correlated to functional outcome but intracranial hemorrhage was not [12]. In that analysis, SD (odds ratio (OR) 0.854; P = 0.02), SV (OR 0.41; P = 0.00), and coefficient of variation (OR 0.572; P = 0.04) of SBP were associated with lower odds of good functional outcome at 3 months (mRS ≤ 2). As in our study, no difference was found between BPV for patients with intracranial hemorrhage versus those without. The studies included in the meta-analysis differed from the present study in several ways: first, regarding the occluded vessels, some studies included extracranial and posterior circulation vessels, whereas others (like our study) did not; secondly, our study, unlike some of the observational studies included in the meta-analysis, was based on pre-defined BP targets and standardized BP data ascertainment; third, some studies included any intracranial hemorrhage while others included only IPH, and whether or not it was symptomatic. Therefore, unfortunately, high degree of heterogeneity in the meta-analysis and the results of our study highlight the uncertainty about BPV as a predictor of both IPH and/or functional outcomes (mRS 0-2) at 90 days.
Several limitations on the present study are worthy of mention. First is the lack of mechanistic justification for the choice of specific indices of BPV utilized. Common statistical measures of variability such as SD and range are more frequently utilized compared to more sophisticated measures such as AVR24, TRI, and SV across this and other studies, which are more rarely used. Their utility and applicability of AVR24, TRI, and SV to AIS, thrombectomy, and their complications remain unarticulated. Furthermore, all indices of BPV are calculated post-hoc, requiring some interval of time for the accumulation of the data and calculation, making them unfit and impractical as treatment targets with current technology at the bedside in the neuro-intensive care unit or emergency department. Another limitation is the mixing of both standard and intensive SBP reduction groups from the BP-TARGET trial. The relationships sought in the present study are those between BPV and outcomes, irrespective of the source of that variability or lack thereof. Nevertheless, there could be differences in those relationships if they were divided into subgroups based on their treatment group assignment in the original trial. There is also the consideration that the topography of ICH has been shown to affect several measures of clinical outcome and the original study did not make a distinction based on where the hemorrhage occurred [20]. Finally, the BP data have an inconsistent time basis and small sample size; the time between measurements varies both systematically due to the design of the trial and at random due to missingness. In our study, we mitigated this by excluding patients with more than 20% missing data, but this only decreases the effect of missing data and comes at the expense of decreasing the sample size. Regardless, our analysis adds to the growing body of literature showing that despite recanalization post-thrombectomy for AIS is associated with decreased BPV, there remains a lack of clear association between BPV and IPH or 90-day independence in this setting. This ultimately underscores the need for further research in this area that may define other biomarkers to improve outcomes.
Conclusions
We observed that full recanalization is associated with decreased BPV post-thrombectomy for AIS. However, we found no evidence that increased BPV is associated with IPH in the 24 h post-procedure or functional independence at 90 days. Our results highlight the need for additional data prior to adoption of reduction in BPV as a therapeutic target post-thrombectomy in AIS patients.
Acknowledgments
The authors would like to recognize the French Health Ministry and the Hopital Fondation A de Rothschild for their support of the creation of the BP-TARGET trial data on which this work was based.
Financial Disclosure
This study was unfunded.
Conflict of Interest
Dr. Walter Merriman has no disclosures to declare. Dr. Adnan Qureshi is cofounder of DyQure, QureVasc, and Qureshi Medica LLC and has received grant support from Chiesi USA. Dr. David Rose has received honoraria/grant funding from Atricure, Boston Scientific, Chiesi, CSL-Behring, Medtronic and Viz. Dr. Mikayel Mazhigi has no disclosures to declare.
Informed Consent
All subjects included in the study on which this work was based were provided with written informed consent.
Author Contributions
Dr. Walter Merriman performed the data analysis and creating the draft of the manuscript. Dr. Mikayel Mazhigi contributed to the conception and the revising of the manuscript for important intellectual content. Dr. David Rose contributed to the analysis of the results and revised the manuscript for important intellectual content. Dr. Adnan Qureshi contributed to the conception, design, and revision of the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AIS: acute ischemic stroke; ARV24: 24-hour average real variability; BPV: blood pressure variability; DBP: diastolic blood pressure; Δ: difference; IPH: intraparenchymal hemorrhage; IV: intravenous; LVO: large vessel occlusion; M1: proximal middle cerebral artery; MAP: mean arterial pressure; mm Hg: millimeters of mercury; mRS: modified Rankin Scale; mTICI: modified Thrombolysis in Cerebral Ischemia; NIHSS: National Institutes of Health Stroke Scale; SBP: systolic blood pressure; SD: standard deviation; SV: successive variability; TRI: time rate index
| References | ▴Top |
- Nogueira RG, Gupta R, Jovin TG, Levy EI, Liebeskind DS, Zaidat OO, Rai A, et al. Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: a multicenter retrospective analysis of 1122 patients. J Neurointerv Surg. 2015;7(1):16-21.
doi pubmed - Mazya M, Egido JA, Ford GA, Lees KR, Mikulik R, Toni D, Wahlgren N, et al. Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: safe Implementation of Treatments in Stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke. 2012;43(6):1524-1531.
doi pubmed - Tanne D, Kasner SE, Demchuk AM, Koren-Morag N, Hanson S, Grond M, Levine SR. Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: the Multicenter rt-PA Stroke Survey. Circulation. 2002;105(14):1679-1685.
doi pubmed - Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, Lees KR, et al. Relationship of blood pressure, antihypertensive therapy, and outcome in ischemic stroke treated with intravenous thrombolysis: retrospective analysis from Safe Implementation of Thrombolysis in Stroke-International Stroke Thrombolysis Register (SITS-ISTR). Stroke. 2009;40(7):2442-2449.
doi pubmed - Butcher K, Christensen S, Parsons M, De Silva DA, Ebinger M, Levi C, Jeerakathil T, et al. Postthrombolysis blood pressure elevation is associated with hemorrhagic transformation. Stroke. 2010;41(1):72-77.
doi pubmed - Berge E, Cohen G, Lindley RI, Sandercock P, Wardlaw JM, Sandset EC, Whiteley W. Effects of blood pressure and blood pressure-lowering treatment during the first 24 hours among patients in the third international stroke trial of thrombolytic treatment for acute ischemic stroke. Stroke. 2015;46(12):3362-3369.
doi pubmed - Mazighi M, Richard S, Lapergue B, Sibon I, Gory B, Berge J, Consoli A, et al. Safety and efficacy of intensive blood pressure lowering after successful endovascular therapy in acute ischaemic stroke (BP-TARGET): a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2021;20(4):265-274.
doi pubmed - Yang P, Song L, Zhang Y, Zhang X, Chen X, Li Y, Sun L, et al. Intensive blood pressure control after endovascular thrombectomy for acute ischaemic stroke (ENCHANTED2/MT): a multicentre, open-label, blinded-endpoint, randomised controlled trial. Lancet. 2022;400(10363):1585-1596.
doi pubmed - Nam HS, Kim YD, Heo J, Lee H, Jung JW, Choi JK, Lee IH, et al. Intensive vs conventional blood pressure lowering after endovascular thrombectomy in acute ischemic stroke: The OPTIMAL-BP randomized clinical trial. JAMA. 2023;330(9):832-842.
doi pubmed - Mistry EA, Mehta T, Mistry A, Arora N, Starosciak AK, De Los Rios La Rosa F, Siegler JE, 3rd, et al. Blood pressure variability and neurologic outcome after endovascular thrombectomy: a secondary analysis of the BEST study. Stroke. 2020;51(2):511-518.
doi pubmed - Al-Salihi MM, Gillani SA, Saha R, Jumaa MA, Zaidi SF, Siddiq F, Gomez CR, et al. Systolic blood pressure reduction strategies in acute ischemic stroke patients following endovascular thrombectomy: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2024;33(7):107724.
doi pubmed - Nepal G, Shrestha GS, Shing YK, Muha A, Bhagat R. Systolic blood pressure variability following endovascular thrombectomy and clinical outcome in acute ischemic stroke: A meta-analysis. Acta Neurol Scand. 2021;144(4):343-354.
doi pubmed - Mazighi M, Labreuche J, Richard S, Gory B, Lapergue B, Sibon I, Berge J, et al. Blood pressure target in acute stroke to reduce hemorrhage after endovascular therapy: the randomized BP TARGET study protocol. Front Neurol. 2020;11:480.
doi pubmed - Gauer OH, Henry JP, Sieker HO. Cardiac receptors and fluid volume control. Prog Cardiovasc Dis. 1961;4:1-26.
doi pubmed - Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, Richart T, et al. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension. 2010;55(4):1049-1057.
doi pubmed - Zakopoulos NA, Tsivgoulis G, Barlas G, Papamichael C, Spengos K, Manios E, Ikonomidis I, et al. Time rate of blood pressure variation is associated with increased common carotid artery intima-media thickness. Hypertension. 2005;45(4):505-512.
doi pubmed - Schachinger H, Langewitz W, Schmieder RE, Ruddel H. Comparison of parameters for assessing blood pressure and heart rate variability from non-invasive twenty-four-hour blood pressure monitoring. J Hypertens Suppl. 1989;7(3):S81-84.
pubmed - https://www.R-project.org/.
- Zhang T, Wang X, Wen C, Zhou F, Gao S, Zhang X, Lin S, et al. Effect of short-term blood pressure variability on functional outcome after intra-arterial treatment in acute stroke patients with large-vessel occlusion. BMC Neurol. 2019;19(1):228.
doi pubmed - Mendiola JMF, Arboix A, Garcia-Eroles L, Sanchez-Lopez MJ. Acute spontaneous lobar cerebral hemorrhages present a different clinical profile and a more severe early prognosis than deep subcortical intracerebral hemorrhages-a hospital-based stroke registry study. Biomedicines. 2023;11(1):223.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.