Role of Serum Biomarkers in the Assessment of Traumatic Brain Injury
DOI:
https://doi.org/10.14740/jnr870Keywords:
Traumatic brain injury, Cranial computed tomography, Glial fibrillary acidic protein, Ubiquitin C-terminal hydrolase L1, Neurofilament light chain, Neuron-specific enolase, S100B protein, Glasgow coma scaleAbstract
Background: Each year, approximately 60 million people suffer a traumatic brain injury (TBI) of varying severity, classified as mild, moderate, or severe. Cranial computed tomography (CT) remains the primary imaging modality of choice for the diagnosis of intracranial lesions, such as hemorrhage or edema, in patients with TBI treated in the emergency department during the acute post-trauma period. CT, combined with patient symptoms and physical examinations, is essential to guide the care of these patients. However, this approach involves exposure to high doses of radiation and requires significant healthcare resources and costs. Furthermore, this diagnostic technique can reveal intracranial lesions in less than 10% of cases of mild-to-moderate TBI. For these reasons, there has been a strong and growing interest in more objective clinical methodologies in the identification of brain lesions, focusing attention on specific biomarkers, i.e. proteins present in the serum closely associated with TBI.
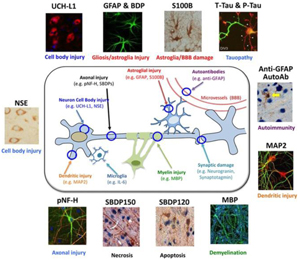
Methods: In this study, some blood biomarkers of TBI, including neuron-specific enolase (NSE), S100B, neurofilament light chain (NFL), ubiquitin C-terminal hydrolase L1 (UCH-L1) and glial fibrillary acidic protein (GFAP) were evaluated in patients who suffered head trauma of different severity, transported to the Emergency and Acceptance Department (D.E.A.) of the “Vito Fazzi” Hospital in Lecce between March 1, 2023 and September 1, 2023.
Results: Based on the diagnostic performances detected on the five tests taken into consideration, GFAP has therefore revealed itself as a potential biomarker to be used in emergency medicine. In fact, since it has not shown any cases of false negative, its high diagnostic sensitivity would allow, for serum values measured within 12 h of mild head trauma lower than the cut-off of 35 pg/mL, to exclude with a good safety margin, patients to be subjected to cranial CT.
Conclusions: Our results support GFAP as a biomarker with the highest negative predictive value in predicting the absence of TBI damage by selecting patients in the emergency department who could avoid performing CT. The application of this study would lead to a significant reduction in patient waiting times in the emergency department and a lower workload for the neuroradiology facility, a reduction in healthcare costs for instrumental investigations and would also avoid unnecessary radiation to the patient.
Published
Issue
Section
License
Copyright (c) 2024 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







