Psychoeducational Therapy and Non-Pharmacological Therapeutic Intervention Approach for Pediatric Epilepsy Neuropsychiatric Comorbidities: A Neuroscience-Informed Strategy for Seizure Management
DOI:
https://doi.org/10.14740/jnr1043Keywords:
Pediatric epilepsy, Seizure, Drug resistant epilepsy, Educational therapy, Psychoeducational therapy, Psychoeducation, Psychiatric comorbiditiesAbstract
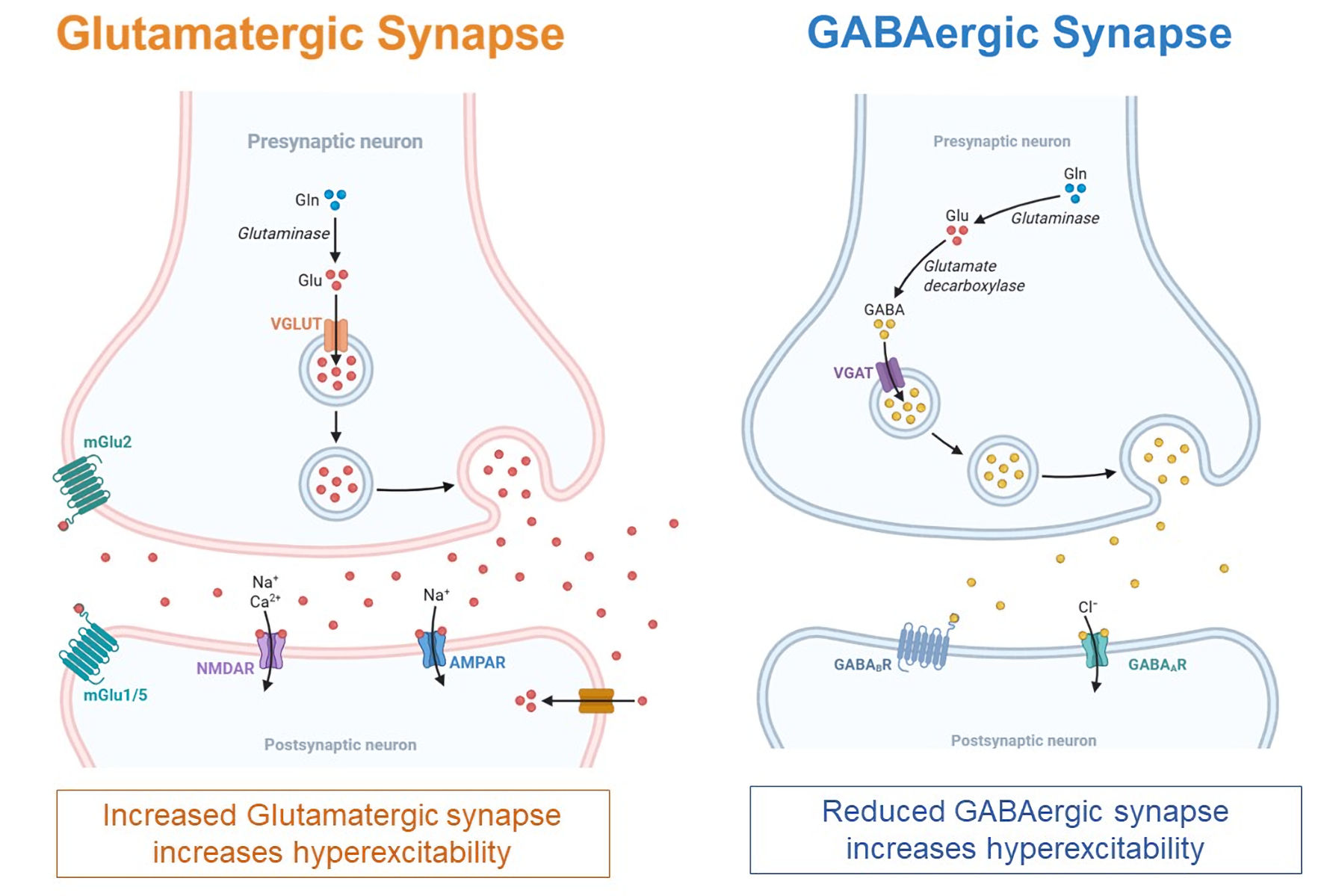
Epilepsy is a prevalent neurological disorder frequently observed in pediatric populations. It affects approximately 0.5% to 1% of population worldwide with higher prevalence in low- and middle-income countries (LMICs). Higher incidence is also observed in children. Pediatric epilepsy is compounded by high rates of neurodevelopmental and psychiatric comorbidities, including attention-deficit/hyperactivity disorder (ADHD), depression, anxiety disorder, obsessive-compulsive disorder (OCD), autism spectrum disorder (ASD), sleeping disorders and learning disorders which negatively affect quality of life, academic achievement, and social integration. These comorbidities demonstrate a complex bidirectional relationship with epilepsy syndromes and may contribute to increased seizure propensity and clinical burden, warranting targeted therapeutic intervention alongside standard epilepsy management. Although pharmacological treatment remains a cornerstone in pediatric epilepsy management, 30% of pediatric patients with epilepsy develop refractory epilepsy (medication resistance). This article aims to synthesize current understanding of neurobiological mechanisms underlying pediatric epilepsy and associated psychiatric comorbidities. It also aims to examine the emerging role of educational and psychoeducational therapies as complementary, non-medication intervention approach to standard pharmacological treatment, and to provide a theoretical framework for integrated care approaches in pediatric drug-resistant epilepsy. Ultimately, a multimodal, family- and school-centered approach integrating pharmacological and non-pharmacological modalities is essential for optimizing long-term outcomes and quality of life in children affected by epilepsy. This narrative review was conducted through systematic literature search of PubMed, Cochrane Library, and International League Against Epilepsy (ILAE) resources from 2020 to 2025, focusing on pediatric epilepsy, psychiatric comorbidities, and non-pharmacological interventions. Search terms included “pediatric epilepsy”, “drug-resistant epilepsy”, “psychiatric comorbidities”, “psychoeducational therapy”, and “educational therapy”. This review presents theoretical frameworks based on existing literature rather than original empirical data. Claims regarding clinical efficacy require further validation through controlled studies.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







