Mortality Following Intracerebral Hemorrhage After Intravenous Alteplase in Acute Ischemic Stroke: A Decision Tree-Based Classification Approach
DOI:
https://doi.org/10.14740/jnr1055Keywords:
Decision trees, Prognosis, Ischemic stroke, Tissue plasminogen activator, X-ray computed tomography, Intracranial hemorrhagesAbstract
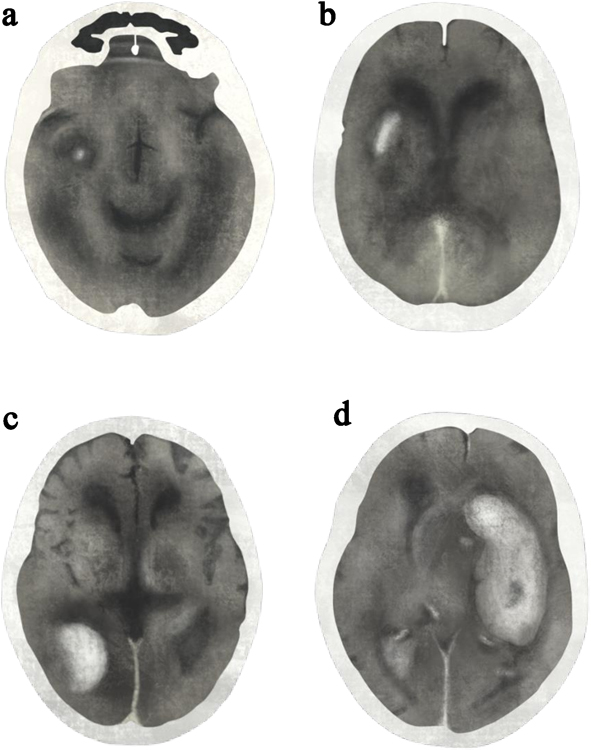
Background: Intracerebral hemorrhage (ICH) after intravenous (IV) alteplase in acute ischemic stroke (AIS) can be assessed clinically as asymptomatic ICH (asICH) or symptomatic ICH (sICH) according to the European Cooperative Acute Stroke Study II (ECASS II) definition, and radiographically as hemorrhagic infarction types 1-2 (HI1-2) or parenchymal hematoma types 1-2 (PH1-2). Reported mortality in sICH ranges from 7.8% to 42.8%, with PH2 carrying the highest risk, up to 50%. Although some patients may benefit from neurosurgical intervention, the prognostic overlap between clinical and radiographic classifications remains unclear. A decision tree approach may clarify mortality risk across subgroups and aid early triage.
Methods: This prognostic descriptive study employed a retrospective cohort design at the Stroke Center, Lampang Hospital. Patients aged ≥ 18 years with AIS who received IV alteplase between January 2017 and December 2024 were included. A decision tree framework was constructed to examine 7-day mortality, incorporating clinical classification, radiographic subtype, and neurosurgical intervention as decision nodes.
Results: Among 94 patients, asICH occurred in 44 (46.8%) and sICH in 50 (53.2%). In the asICH group, HI2 was the predominant subtype (24/44, 54.6%) and all survived. In the sICH group, PH2 was the leading subtype (30/50, 60.0%). Mortality was influenced by surrogate compliance with neurosurgical advice: refusal of surgery after recommendation resulted in 100% mortality, whereas acceptance reduced mortality to 43.8% (P = 0.043).
Conclusion: Post-alteplase ICH had a 7-day mortality of 27%. The decision tree framework offered a simple visualization for early risk stratification and may help support clinical decision-making.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







